Vaping FAQs
.
Last updated 21 September 2024
.
Other useful resources
- Mendelsohn CP, Wodak A, Hall W, Borland R. Evidence review of nicotine vaping and recommendations for regulation in Australia. 23 October 2023
- Vaping myths and the facts. National Health Service, UK 2023
- Vaping to quit smoking. National Health Service. UK 2023
- Vaping Facts website. New Zealand Ministry of Health
- Addressing common myths about vaping. Action on Smoking and Health UK, 2023
- Vaping: a guide for health and social care professionals. UK National Centre for Smoking Cessation and Training 2023
- Evidence summaries from Clive Bates on 1) Safety 2) Effectiveness 3) Youth use 4) Policy
The basics
Tobacco Harm Reduction is a strategy to reduce the harm for smokers who are unable or unwilling to quit. It involves replacing high-risk combustible tobacco products such as cigarettes with lower-risk, non-combustible nicotine alternatives, like vaping.
Video: Introduction to Tobacco Harm Reduction, March 2022 (10 mins)
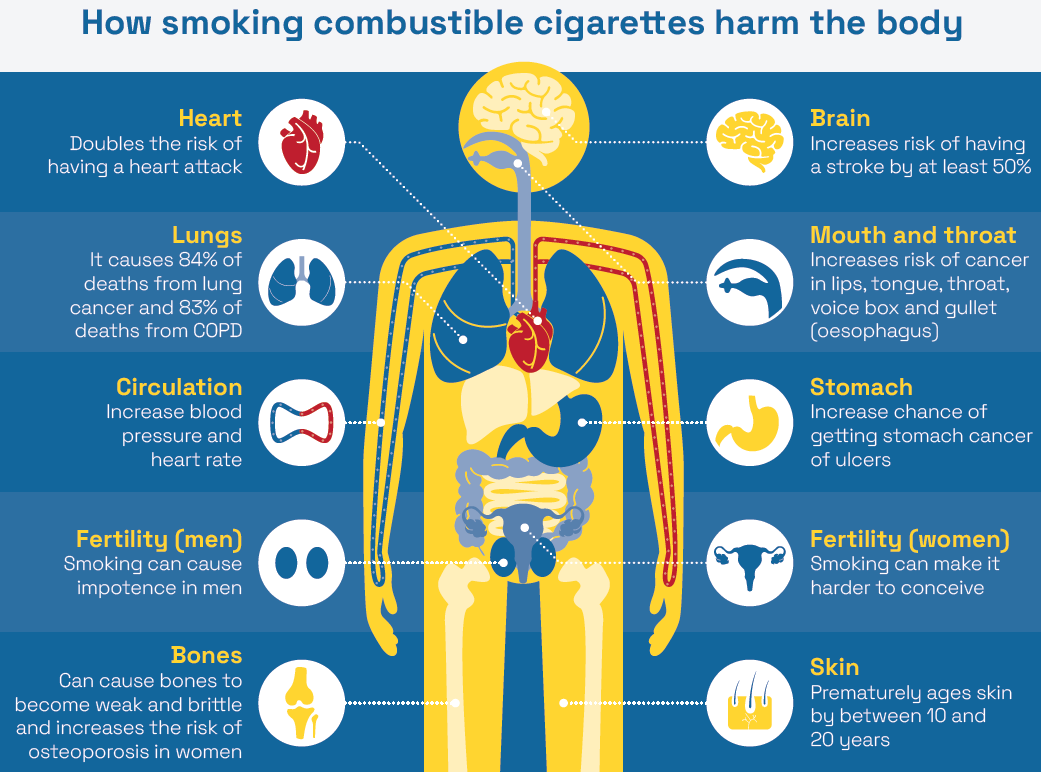
The aim of harm reduction is to reduce (not necessarily eliminate) the harms from smoking, in particular cancer, heart and lung disease. The aim is not to stop nicotine as nicotine causes little harm. Almost all the harm from smoking is from the thousands of toxic chemicals and carcinogens (cancer-causing chemicals) from burning tobacco. Reduced-risk products are not risk-free, but they are far safer than smoking.
Reduced-risk nicotine products fall on a ‘continuum of risk’. They include vaping (using an e-cigarette), Swedish snus (small pouches of special tobacco placed under the upper lip), nicotine pouches (similar to snus but without tobacco) and heated tobacco products (which heat tobacco without burning it).
The aim of tobacco harm reduction is for nicotine users is to shift from deadly combustible products on the right of this diagram to safer products on the left.
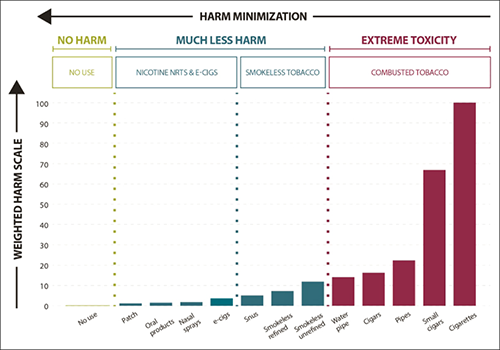
The harm continuum of nicotine products (safer products on the left)
Safer nicotine products can supplement traditional tobacco control strategies which target complete quitting.
Tobacco harm reduction is no different to other harm reduction strategies which are generally very effective and widely accepted. These include methadone for heroin users, clean needle exchange programs and even car seat belts.
Tobacco harm reduction is one of the three pillars of Australia’s National Tobacco Strategy. One objective of the NTS is to “reduce harm associated with continuing use of tobacco and nicotine products” (p11).
Australia is legally obligated to support tobacco harm reduction as a signatory to the World Health Organisation Framework Convention on Tobacco Control. The FCTC provides an obligation on governments to not only allow reduced-risk products but actively promote them as part of implementing their tobacco control policies. Currently Australia is in breach of its international obligations as no harm reduction strategies are supported in practice.
Vaping is a less harmful alternative for adult smokers who are unable to quit smoking on their own or with other methods. Vaping delivers nicotine and mimics the familiar hand-to-mouth action, habit and sensations of smoking.
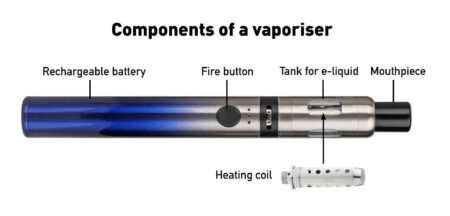
Nicotine vapes (e-cigarettes, vaporisers, ENDS) heat a liquid nicotine solution into an aerosol which is inhaled and exhaled as a visible mist. This is known as ‘vaping’.
All vapes consist of a battery (usually rechargeable), a tank or pod to hold the e-liquid and a coil or heating element to heat the liquid to create the vapour.
As there is no tobacco and no combustion, almost all the toxic chemicals in smoke are absent from vapour. Those that are still present are in far lower doses than in tobacco smoke.
Some smokers use vaping for a short time to quit tobacco smoking and then cease vaping. Others continue vaping long-term to prevent relapse to smoking. Some smokers experiment with vaping without intending to quit but then ‘accidentally’ quit.
Vapers take about 220 puffs per day on average [Yingst 2020 172; Aherrera 2020: 365; Dautzenberg 2015: 163; Kosmider 2019: 156; Dawkins 2013: 236; Robinson 2015: 225]. Some vapers takes vaping breaks of 10-12 puffs at a time. Others prefer to “graze” through the day, taking one or two puffs as needed. Either method is fine.
Inhalations from vaping are typically longer than when smoking: typically 3-4 seconds compared to 1-2 seconds.
Vaping should not be used by non-smokers including young people who don’t smoke.
Most people who take up vaping are smokers trying to reduce their risk of harm from smoking.
In Australia in 2023, current smokers aged 14+ gave the following reasons for taking up vaping (could select more than one response) according to the 2023 National Drug Strategy Household Survey: (Table 3.37)
- To quit smoking 36%
- To reduce smoking 28%
- They taste better 27%
- They are cheaper 25%
- To prevent relapse to smoking 22%
- Because they are less harmful 22%
- 42% of smokers said curiosity was a factor in their decision to try vaping
In Great Britain, ASH found similar results in 2023. The 4 main reasons for vaping were
- To quit smoking 31%
- To prevent relapse 17%
- Because they enjoy the experience 14%
- To save money compared to tobacco 11%

In the latest national survey, 1.5 million Australians, or 7% of the adult population (14+) vaped at least monthly and 3.5% vaped daily. In comparison, 1.8 million Australians, or 10.5%, adults smoke and 8.6% smoke daily. (National Drug Strategy Household Survey 2022-23)
Another survey by Roy Morgan, reported in January 2024 that there were 1.7 million adult (18+) vapers in Australia, or 8.3% of the population. The number of people vaping had grown by 349% in 5 years.
Comparison with other Western countries
Despite the harsh restrictions on vaping, Australia now has one of the highest adult vaping rates in the world.
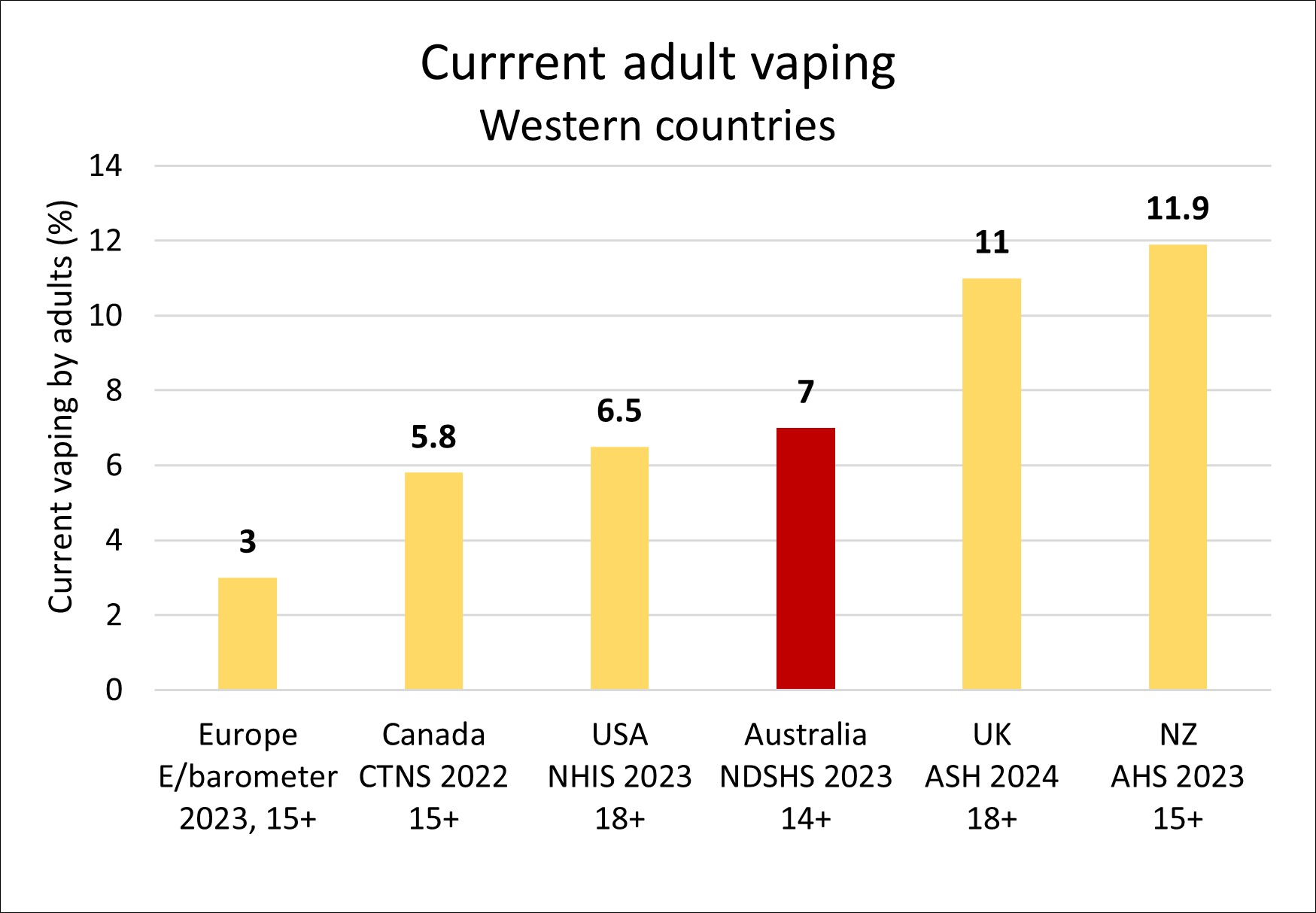
- New Zealand, 11.9% (vaping monthly, 15+, 2023)
- Great Britain, 11% (current vaping, 18+, 2024)
- USA, 6.5% (vaping every day or some days, 18+, 2023)
- Canada, 5.8% (15+, past month, 2022)
- Europe, 3% (current vaping, 15+, 2023)
You can vape legally in Australia with a nicotine prescription from a doctor
Currently only 8% of Australian vapers have a nicotine prescription. The prescription model is a significant barrier for adult smokers wishing to legally access regulated nicotine vaping products to quit smoking or to reduce smoking-related harm.
Most doctors are reluctant to prescribe nicotine. As of April 2023, there were only 1963 doctors authorised to prescribe nicotine out of >100,000 doctors in Australia However only about 500 are publicly listed. The RACGP recommends that prescriptions are for 3 months only, although they can be up to 12 months supply.
The prescription model has led to a lucrative, thriving black market run by organised crime groups, selling unregulated, mislabelled, high nicotine content disposable vapes to adults and children.
There are severe penalties (up to $45,000 and up to two years jail) for using or possessing liquid nicotine unless it is prescribed by a doctor to help you quit or cut down smoking.
| State | Penalty | Prison Term | Legislation |
| ACT | $32,000 max or prison or both | 2 years | Medicines, Poisons and Therapeutic Goods Act 2008, 4.1.3, 36 |
| Western Australia | $45,000 | Medicines and Poisons Act 2014, 2.16.2 and 115 | |
| Victoria | $1,817 | Drugs, Poisons and Controlled Substances Regulations 2017 | |
| South Australia | $10,000 max | Controlled Substances Act 1984, 4.22 | |
| Northern Territory | $15,700 max or prison | 12 months | Medicines, Poisons and Therapeutic Goods Act , 2.2, Div 3, 44.2 |
| Queensland | $27,570 max | Medicines and Poisons Act 2019 , 2.1.1.34 | |
| New South Wales | $2,200 max or prison or both | 6 months | Poisons and Therapeutic Goods Act 1966, No 31, 16 |
| Tasmania | $8,650 or prison | Up to 2 years | Poisons Act 1971, Part 3, Division 1, Clause 36 |
State and Territory laws regulate issues such as sale, use in public places, age limits on sale, display and promotion of vapes.
The only legal way to purchase vapes is from an Australian pharmacy with a doctor’s prescription. Nicotine cannot be sold legally in Australia by vape shops, tobacconists or other retail outlets.
You will need to inform your doctor which product, brand and flavour (tobacco, mint or menthol) you require and find an Australian pharmacy that can provide it. The volume supplied per script is not limited, but is determined by the doctor.
However, there are only a very small number of community and online pharmacies which stock nicotine vaping products and most stock a very small range
There are additional standards for products supplied by pharmacies, including a full ingredient list, labelling, packaging regulations, safety warning statements and child-resistant containers. Nicotine concentrations up to 100mg/mL can be sold by pharmacies if approved by your doctor.
See below under “Regulation of Vaping” for more.
Safety and health
Vaping is not risk-free but it is far less harmful than smoking which kills up to two in three long-term users.
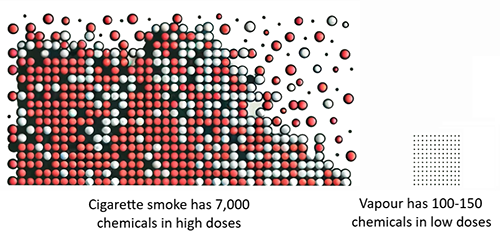
Almost all the harm from smoking is caused by the 7,000 chemicals in smoke (including 70 cancer-causing agents) released from burning tobacco. (Khouja 2024)
Source: No Smoke Less Harm 2024 (here)
In contrast, vapes heat a liquid into an aerosol, without tobacco, combustion or smoke. The toxic constituents in smoke are either absent in vapour or, if present, are mostly at levels significantly below 5% (mostly below 1%) of doses from smoking and far below safety limits for occupational exposure. and are at generally at much lower levels than in cigarette smoke. Studies have found on average around 100-150 chemicals in vapour from an individual device (eg Heywood review; Sleiman: Margham).
A comprehensive systematic review in 2022 for England’s Office for Health Improvements and Disparities concluded:
“Vaping poses only a small fraction of the risks of smoking and is ‘at least 95% less harmful’ than smoking”
According to the UK Royal College of Physicians report in 2024:
“Vaping exposes vapers to a far narrower range of toxins than does smoking cigarettes, and levels of toxins absorbed from vaping are generally low. It is therefore likely that vaping poses only a small fraction of the risk of smoking”
A review by the US National Academies of Sciences, Engineering and Medicine in 2018 concluded:
“While e-cigarettes are not without health risks, they are likely to be far less harmful than combustible tobacco cigarettes”
The advice of the United Kingdom National Health Service is:
“Nicotine vaping is not risk-free, but it is substantially less harmful than smoking”
According to the UK National Centre for Smoking Cessation and Training:
“Anyone who switches from smoking to vaping is instantly improving their current and future health”
Numerous studies have also shown substantial reductions in biomarkers of exposure (toxins in the blood, saliva or urine of users) and biomarkers of potential harm (signs of damage to the body) in tobacco smokers who have switched to vaping.
Individuals who use nicotine vapes to quit smoking completely will gain significant health benefits. Clinical trials and surveys of smokers who completely switched to e-cigarettes have shown improvements in asthma, chronic obstructive pulmonary disease (COPD), blood pressure, muco-ciliary clearance, respiratory infections, lung function, respiratory symptoms, cardiovascular markers and gum disease.
Based on the level of carcinogens and their potency, the lifetime cancer risk from vaping has been estimated as less than 0.5% of the risk from smoking.
For a review of the evidence on vaping safety please watch my presentation to the National Drug and Alcohol Research Centre at the University of New South Wales [17 February 2022]:
A written summary of the presentation is also available here.
Common side-effects
The side-effects most often reported from vaping are throat or mouth irritation, headache, cough and feeling sick. According to the Cochrane review the side-effects “appeared similar to those people experience when using NRT” (up to 2 years follow-up). These tend to reduce over time as people continue vaping. Another review of 18 studies did not find a difference in the rate of side effects between vaping nicotine and nicotine replacement products.
Is vaping safe?
Much of the debate about vaping is framed in terms of whether vaping is safe. This is the wrong question and sets a high bar that we do not apply to other behaviours, such as drinking alcohol, eating fast food, or playing sport.
Nothing is completely safe. We all take risks every day, weighing the risks against the benefits. We decide if the risks are within our ‘risk appetite’ for the benefits we get.
Nicotine products fall on a continuum of risk with the most harmful products being combusted tobacco. E-cigarettes containing nicotine are at the lower end of the scale and cause little harm in comparison.

Nicotine risk continuum (adapted from Abrams 2020)
Reducing your risk
If you vape, you can reduce your risk further:
1. Avoid vaping at excessively high temperatures to reduce the production of toxic byproducts. (PHE 2018)
2. Vape with higher concentrations of nicotine. If the nicotine concentration is too low, you will compensate by puffing more and will inhale more toxicants. (Dawkins 2016)
3. Use high quality, reputable products to reduce exposure to contaminants (remember EVALI). (Mendelsohn 2022)
4. Unflavoured vapes avoid exposure to flavouring chemicals whose long-term effects are unknown.
5. Cease vaping when you are confident you won’t relapse to smoking.

Yes. This estimate is based on comprehensive, independent reviews of the scientific evidence.
The most rigorous and comprehensive systematic review of the health effects of vaping nicotine commissioned by the England government (Office of Health Information and Disparities) in 2022 concluded
Vaping is “at least 95% less harmful” than smoking, based on their finding that “vaping poses only a small fraction of the risks of smoking”
The same conclusion was reached by both Public Health England and the UK Royal College of Physicians, who put it this way:
“Although it is not possible to precisely quantify the long-term health risks associated with e-cigarettes, the available data suggest that they are unlikely to exceed 5% of those associated with smoked tobacco products, and may well be substantially lower than this figure”
Of course, the exact figure doesn’t really matter, but saying the risk of vaping is probably less than 5% of smoking helps to communicate a ballpark for the level of risk so smokers can make an informed choice. Just saying vaping is ‘less harmful’ is too vague. That could be 30%, 60%, or maybe even 99% less harmful.
The ”95% safer” figure is based on the following evidence
- Most of the harmful toxicants in smoke are completely absent from vapour. Those that are present are at much lower concentrations, mostly at levels below 1% of what they are in smoke. If the toxins are much lower, the health risks will be much lower.
- When smokers switch to vaping, levels of toxicants and carcinogens (biomarkers of exposure) measured in the blood, saliva and urine are substantially lower and for many toxins are the same as for a non-smoker.
- Smokers who switch to vaping also have lower levels of biomarkers of potential harm, ie changes in the body from smoking that are associated with disease eg oxidative stress, inflammation, endothelial dysfunction
- There are substantial health improvements in smokers who switch to vaping. Risk of a heart attack reduces, the blood pressure falls, asthma and COPD (emphysema) improve and smokers often say they just feel a lot better after switching.
- The risk of cancer from vaping has been independently estimated to be <0.5% of the risk from smoking.
- After 15 years of vaping nicotine in dozens of countries, there has not been one death. Serious health effects are extremely rare.

Like all new products, the long-term risk of using e-cigarettes will not be fully understood for some years. However it is highly likely vaping will be considerably less harmful than smoking. [OHID UK, NASEM, COT UK, PHE, NZMoH, Health Canada]
Vaping is not risk-free. However, the risk must be compared to the alternative, i.e., continuing to smoke. Based on scientific principles and what we already know (which is substantial), the Royal College of Physicians estimates the long-term risk is likely to be no more than 5% of the risk of smoking.
According to Professor Ann McNeil, author of the UK government commissioned reviews on the harms of vaping,
“It is wrong to say we have no idea what the future risks from vaping will be. On the contrary levels of exposure to cancer-causing and other toxicants are drastically lower in people who vape compared with those who smoke, which indicates that any risks to health are likely to be a fraction of those posed by smoking”
In the absence of long-term data, modelling studies are a well-accepted way of estimating the population impact of an intervention. Numerous modelling studies estimate that vaping nicotine has a significant net public health benefit under all realistic assumptions and would do so even if it generated 20% of the harm of smoking.
Given that it appears to take in the vicinity of 20 years or more of daily smoking to increase risk of premature mortality, taking in a fraction of that amount over similar periods is likely far less likely to produce adverse effects.
There were an estimated 82 million people vaping in dozens of countries in 2021. Some ex-smokers have used vapes for over a decade, and to date, reports of serious adverse effects are very rare.
The requirement for policy to wait decades for evidence of long-term safety is not applied to other medical or consumer product, for example COVID vaccines. We normally base decisions on the current evidence and modelling studies. Nicotine vaping devices have been used by millions of consumers for far longer than many approved medicines or consumer products.
There is a theoretical possibility that long-term vaping may increase the risks of lung cancer, emphysema, cardiovascular and other smoking-related diseases. However, these risks are likely to be significantly lower than the risks of smoking and low in absolute terms.
Like all new medicines and treatments, post-market surveillance of vaping (ongoing monitoring after going on the market) should continue to monitor safety and detect any new side-effects. As with any new product, it is possible that some harms may emerge over time.
If cigarettes were invented today, we would know very quickly that they were very, very harmful.
We know much more today about chemistry, toxicology, physiology and the causes of disease than when cigarettes were introduced over a century ago. We have a much greater understanding of the toxic effects of most chemicals and can assess them against occupational and environmental health and safety standards. The scientific method, analytical techniques and equipment are also far superior to that available in the past.
This claim is a tactic by vaping opponents to cast doubt on the safety of vaping. However, extensive and rigorous research of vapes has concluded beyond reasonable doubt that vapes carry only a small fraction of the risk of cigarettes and are a far safer substitute for smoking.
The requirement to prove long-term safety when a product is launched is not applied to any other product. Regulators require safety data but do not ask for decades of epidemiological evidence before approving a new medicine. The COVID vaccine was approved within a few months. Like vaping, delaying it would inevitably result in many preventable deaths from COVID and is not justified. Similarly, delays in making vapes available would lead to huge numbers of unnecessary deaths from smoking.
Post-market surveillance is available to identify any unexpected adverse effects that may arise.
Switching from smoking to vaping dramatically reduces your risk of cancer. And, in spite of what many people think, nicotine does NOT cause cancer.
Presentation on the relative risk of cancer from smoking and vaping,
Medical Grand Rounds, Prince of Wales Hospital, Sydney, 22 November 2023
The overall cancer risk from vaping nicotine is estimated to be <0.5% (less than one in two hundred) of the risk from smoking. The lung cancer risk has been estimated to be 50,000 times less than from cigarette smoking. The lifetime lung cancer risk fromsecond-hand vapouris estimated to be 50,000 times less than from second-hand smoke.
This is because the cancer-causing chemicals (carcinogens) in tobacco smoke are dramatically reduced in vapour. According to the International Agency for Research on Cancer and the US Surgeon General, the main cancer-causing toxins in tobacco smoke are:
- polycyclic aromatic hydrocarbons
- tobacco-specific n-nitrosamines
- volatile organic compounds (Benzene; 1,3-butadiene)
- aldehydes (formaldehyde, acetaldehyde)
- aromatic amines (2-naphthylamine; 4-aminobiphenyl
- ethylene oxide
When smokers switch to vaping all of these carcinogens are substantially reduced, when measured in the body fluids. In many cases they are at the same level as a non-smoker. Ensuring you do not vape at an excessively high temperature reduces the production of toxicants and the health risk further. (PHE 2018)
Contrary to popular belief, nicotine itself does not cause cancer. (International Agency for Research on Cancer; USDHHS 2010)
Expert opinion
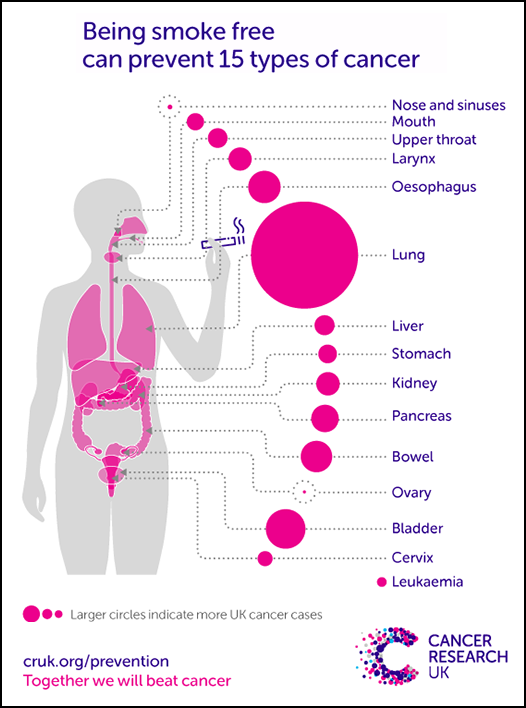
Vaping is strongly supported by the leading UK cancer charity Cancer Research UK, which states:
“There is no good evidence that vaping causes cancer. Because vaping is far less harmful than smoking, your health could benefit from switching from smoking to vaping. And you will reduce your risk of getting cancer”
A review by the US National Academies of Sciences Engineering and Medicine concluded:
“There is little evidence that e-cigarettes pose significant cancer risk”
UK National Centre for Smoking Cessation and Training
“The cancer risk for people who vape is considerably lower than for those who smoke”
Cancer from smoking
Smoking is responsible for 21% of the total cancer burden in Australia and 65% of this is due to lung cancer. Smoking is predicted to cause over 250,000 cancer deaths in Australia from 2020 to 2044.
Tobacco smoke contains 69 known carcinogens and causes at least 15 types of cancer.
Further reading: Switching from smoking to vaping dramatically reduces cancer risk
Unlike secondhand smoke, there is no evidence that passive vaping is harmful to bystanders.
According to expert health organisations:
- Public Health England’s review in 2018. “To date there have been no identified health risks of passive vaping to bystanders”
- Health Canada in 2023. “The risks [from second-hand vapour] are expected to be much lower compared to second-hand smoke from a tobacco product. This is because second-hand aerosol from vaping contains significantly fewer chemicals than cigarette smoke.”
- UK National Health Service, 2023. “There is no evidence so far that vaping is harmful to people around you”
Chemical exposure. Research shows that vaping releases extremely low levels of chemicals into the surrounding air which pose very little risk to health. In one study, a range of of toxins were tested in bystanders None were increased except for IL-1B levels (a sign of inflammation), possibly due to secondhand exposure. Bystanders are exposed to low levels of chemicals because:
- The person vaping absorbs over 90% of the inhaled aerosol – less than 10% of the chemicals are exhaled
- About 85% of secondhand smoke comes from sidestream smoke released from the burning tip of the cigarette, but there is no sidestream vapour released from vaping products
- The liquid aerosol droplets from vapour evaporate and disperse in seconds, much more quickly than the solid particles in smoke, reducing risk further.
Nicotine levels in the air from vaping are also very low. A 2024 real-world US study found that children absorbed 16% of the nicotine from indoor vaping compared to smoking. This confirmed the finding of an earlier study which found that exposure to nicotine in children was 12% compared to tobacco smoke. Another study found that, nicotine levels from secondhand vapour were marginally raised, but were unlikely to cause dependence.
Cancer risk. Based on the carcinogens in second-hand vapour and the estimated doses, the cancer risk for passive smokers was estimated to be five orders of magnitude (50,000x) greater than for passive vapers.

Nicotine is a relatively benign drug. Although it causes dependence, it presents very little risk to the user and even has some significant beneficial effects.
Because of its association with smoking, many people incorrectly believe it is the harmful ingredient in tobacco smoke. However, the vast majority of harm from smoking comes from tar, carbon monoxide, toxic gases and solid particles released by burning tobacco, not from the nicotine.
Expert assessment of nicotine risks
- UK Royal College of Physicians 2024, “There is little evidence of a long-term harmful physiological effect of nicotine” and “most of the harm from smoking is caused by [these] products of combustion” (page 8).
- The Royal Society for Public Health has concluded that nicotine is a mild recreational stimulant and is “no more harmful to health than caffeine”
- Public Health England “nicotine use per se represents minimal risk of serious harm to physical health and that its addictiveness depends on how it is administered”
- UK National Health Service, “Although nicotine is addictive, it is relatively harmless to health. Nicotine itself does not cause cancer, lung disease, heart disease or stroke”
- Professor Neal Benowitz: “Nicotine plays a minor role, if any, in causing smoking-induced diseases”
- 15 past presidents of the Society for Research on Nicotine and Tobacco (SRNT): “Nicotine is the chemical in tobacco that fosters addiction. However, toxic constituents other than nicotine, predominantly in smoked tobacco, produce the disease resulting from chronic tobacco use”
Nicotine does not cause cancer
- International Agency for Research on Cancer (IARC) 2012: “nicotine is not carcinogenic” (p139)
- US Department of Health and Human Services 2014: There is insufficient data to conclude that nicotine causes or contributes to cancer in humans” (Ch5, p116)
- Royal College of Physicians 2016: “nicotine alone is not carcinogenic” (p58)
- US National Academies of Sciences, Engineering and Medicine (NASEM) 2018: “there is no human evidence to support the hypothesis that nicotine is a human carcinogen” (p4-17)
- Cancer Research UK 2023: “nicotine does not cause cancer”
- Health Canada 2023: “nicotine itself is not known to cause cancer”
Health effects of nicotine
Nicotine has mild effects such as temporarily increasing the pulse and blood pressure and narrowing the blood vessels. It can impair wound healing and raise blood glucose levels.
Nicotine does not cause lung disease or stroke, and only has a minor role in cardiovascular health (Benowitz: Kim).
Long-term use of nicotine is regarded as low-risk, based on decades of use of Swedish snus which releases high levels of nicotine, and nicotine replacement therapy. Nicotine in nicotine replacement therapies such as nicotine patches and gum is on the WHO List of Essential Medicines. Nicotine is approved for use as a medicine in Australia from the age of twelve.
Beneficial effects of nicotine
Nicotine has a range of benefits, including hedonistic (pleasure), functional and therapeutic effects:
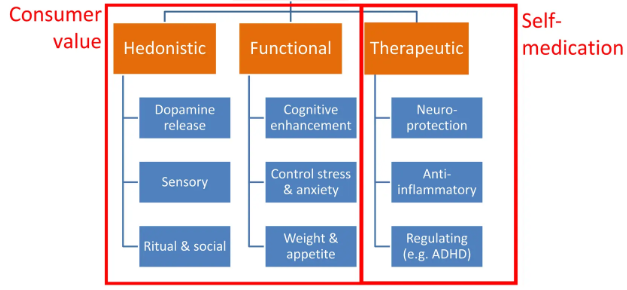
Source: Clive Bates, ECig Summit 2023
- Nicotine improves attention, working memory and cognitive function (more here)
- It also creates pleasure, reduces anxiety and relieves depression
- Therapeutic effects on Parkinson’s disease, schizophrenia, ulcerative colitis and attention deficit disorder
- Weight control
- Pain relief
Many people regard nicotine (when delivered with minimal harm) as a socially acceptable recreational stimulant, like caffeine and alcohol.
A word on the definition of ‘addiction’
The urge to vape is not strictly characterised as “addiction”. According to Addiction Ontology, the definition of addiction is a compulsion to engage in a behaviour known to cause serious net harm.
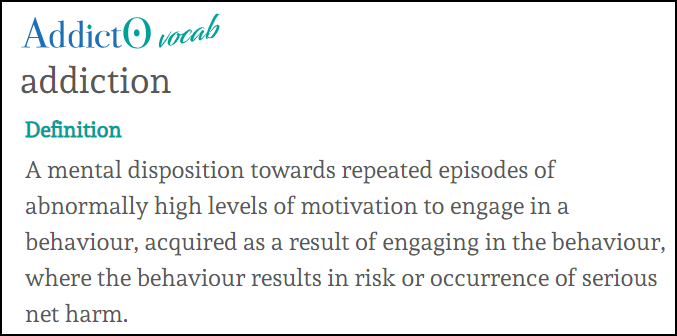
Nicotine has only minor health effects and the urge to vape is best described as dependence. Dependence means having the urge to use a drug to avoid physical symptoms of withdrawal when it is ceased.
The dependence of nicotine alone is also overrated. There are other ingredients in tobacco smoke which make nicotine more habit-forming (monoamine oxidase inhibitors). Cigarettes also deliver nicotine very quickly which increases its dependence potential.
However, outside of tobacco smoke, nicotine is far less dependence-forming. For example, nicotine gum and patches have very low risk of dependence but are used long-term by some ex-smokers to prevent relapse. The behavioural, sensory and social aspects of smoking also enhance dependence.
A double standard: nicotine and caffeine
Nicotine dependence is often met with outrage and alarm, while caffeine dependence is largely dismissed as a minor concern. Caffeine dependence is generally accepted as a small price to pay for the enjoyment and perceived benefits of its use, with little of the stigma attached to nicotine.
Like nicotine, caffeine has stimulant and cardiovascular effects and similar withdrawal symptoms to nicotine. (Denaro 1991) People have died from overdoses of caffeine (Capelletti 2018)) as well as nicotine. (Maessen 2020)
Caffeine is the most widely used psychoactive drug in the world. Many regular coffee drinkers experience withdrawal symptoms strikingly similar to those of nicotine withdrawal when they miss their daily dose. It’s common to hear people say they “can’t start the day” without a coffee. Neither drugs should be used by young people.

There is no evidence that nicotine vaping causes seizures. The fact that a seizure occurred while vaping or soon after, does not prove that vaping was the cause.
A study in 2019 found that 114 vapers had reported a seizure. However this observational study could not indicate whether vaping had caused the seizures. In the US, 35 cases of seizures ‘associated with vaping’ were reported to the FDA from 2010-2019.
Soon after, the FDA acknowledged that “A causal relationship between e-cigarette use and seizure has not been established“. Some of these episodes were in people with epilepsy, others caused by illicit drug use.
Further, a review of vaping and seizures in 2020 by Professor Neal Benowitz:
Did “not consider seizures to be a potential adverse effect that should influence the decision of an adult smoker to use e-cigarettes to try to stop smoking conventional cigarettes”
Nevertheless, claims that vaping causes seizures are breathlessly reported by the media. It is also claimed without evidence in Australian government-commissioned reports eg here and here.
Association or causation?
Both vaping and seizures are common
- About 1.6 million adult Australians and many young people are currently vaping.
- At least 150,000 Australians are estimated to have seizures from epilepsy. Other causes are medications, drug and alcohol use, a head injury, a brain tumour or brain infection.
As a result, it is likely that some people who vape will have a seizure from time to time. However, this is an association of two behaviours, and is not causal.
The NHMRC incorrectly claims that there is “high certainty” evidence that vaping leads to seizures. This claim was subsequently debunked by 11 leading international experts in a critique in Addiction:
“A small number of case studies have reported seizures in people using nicotine e-cigarettes, but these cases do not establish causation and hence do not qualify as ‘high-certainty’ evidence. Many of these cases had a pre-existing seizure disorder, and some had used other drugs. If nicotine e-cigarette use was a cause of seizures, an association between cigarette smoking and seizures would also be expected—but none has been reported”
Severe nicotine poisoning
Claims of seizures from vaping nicotine may be confused with seizures from severe nicotine poisoning. A nicotine overdose from ingesting nicotine liquid can cause seizures and this may have led some people to think that nicotine vaping may also be implicated.
Further reading: Benowitz N. Seizures after vaping nicotine in youth: A canary or red herring J Adol Health 2019
Research has not identified any serious harms to the lungs from vaping nicotine in the short-medium term. An expert review concluded that vaping nicotine is unlikely to raise any significant concerns for lung health. (Polosa)
Improved lung health after switching from smoking
There is good evidence that lung health improves in smokers who switch to vaping. Breathing, cough and reduced phlegm improve (Hajek; Shiffman) and there are short- to medium-term improvements in asthma (Polosa), chronic obstructive pulmonary disease (emphysema) at 5-year follow up (Polosa), muco-ciliary (phlegm) clearance (Polosa), respiratory infections (Miler; Lucchiari) and lung function (Cibella). These changes are likely to persist over the longer term. Furthermore, the lung cancer risk from vaping is estimated to be 50,000 times less than from smoking. (Scungio)
Harm from vaping by non-smokers
Longitudinal studies in people who have never smoked have not found significant harmful effects so far on lung health.
- Non-smokers may get transient throat irritation, cough or wheeze. However, there is no evidence to suggest that this may lead to clinically significant harm. (Polosa)
- A 2-year longitudinal study in 2024 by Karey found “no significant association … between e-cigarette use [in never-smokers] and important respiratory symptoms”. In a similar study, Reddy also found no increase in respiratory symptoms after 12 months in never-smokers who vaped.
- A 2-year study by Sargent found that “no significant association was detected between e-cigarette use and important respiratory symptoms”, concluding that respiratory symptoms were “largely not significantly different from never or former tobacco users”.
- Polosa studied nine daily vapers who had never smoked and found no evidence of lung damage after 3.5 years. There were no respiratory symptoms, no changes in lung function, markers of inflammation or change in lung scans.
- Kenkel found no evidence of respiratory disease in a longitudinal study over 3-years of 12 never-smokers who vaped.
- Sanchez-Romero found that exclusive vaping in never-smokers did not increase the risk of wheezing in a national study over 5 years in the US. However an increase in wheezing was reported in smokers.
- Berlowitz reported a reduction in cough but found an increase in wheezing in non-smoking vapers. The significance of the results has been questioned because of the low numbers, reliability of self-reports, possible other explanations and uncertain clinical significance.
However, larger, longer studies are needed before firm conclusions can be drawn. There may be some risk for heavy, long-term vapers.
Contrary to media reports, vaping nicotine does not cause the serious lung disease EVALI (Mendelsohn), “popcorn lung” (CRUK) or spontaneous pneumothorax.
This review does not include cross-sectional studies which cannot determine causation.
See below for more about the effects of vaping in young people.
What about laboratory studies?
Cell and animal studies have found that vaping can cause oxidative stress, inflammatory changes, reduced cell viability (survival) and DNA damage, although these changes are much less than from smoking. (Wang; Caruso; Emma) Findings from cell and animal studies are often not a reliable guide to human effects and should be treated with caution. (Bracken)
Conclusion
Vaping is not risk-free and it is not recommended for non-smokers. However, vaping is clearly far less harmful to the lungs than smoking because of the substantial reduction in exposure to toxins. The research so far has not found significant concerns to the lungs from short-medium term use.
Nevertheless, it is possible that respiratory harm from vaping may become apparent from many years of use, especially in long-term and heavy users, and continued investigation is needed.
Acknowledgement
Thank you to Professor Riccardo Polosa for reviewing this analysis.

No. This condition was not caused by nicotine vaping.
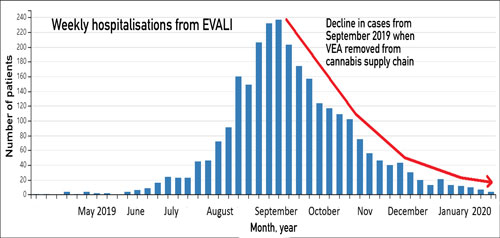
In 2019, there was an outbreak of a serious lung injury EVALI (E-cigarette, or Vaping, product use-Associated Lung Injury) in the US in people who had recently vaped. This condition has now been clearly associated with vaping black-market cannabis (THC) oils contaminated with vitamin E acetate (VEA), purchased from street dealers.
Not a single case has been linked to commercial nicotine vaping to stop or reduce smoking. VEA cannot be dissolved in nicotine e-liquid and has never been detected in nicotine e-liquid. Noo other potential cause in nicotine vapes has been identified.
When VEA was removed from the illicit supply chain, EVALI disappeared in early 2020. No further cases have been reported in the US despite the continuing widespread use of nicotine vaping and no significant e-cigarette product changes.
Some fourteen percent of cases denied using THC vapes and some commentators have incorrectly claimed that nicotine vapes must have been the cause. However some of those who denied using THC were later found to have done so after family interviews or testing. Also, THC was illegal in many states at the time. False denials were more common in states where THC was illegal.
The death of an Australian man in 2021 was incorrectly attributed to EVALI. The man had been a heavy smoker for 40 years and switched to vaping 10 years before his death. It is far more likely that the man died from progressive lung damage caused by 40 years of heavy smoking.
 No. There is no evidence that vaping nicotine causes this condition and there has never been a single case linked to vaping.
No. There is no evidence that vaping nicotine causes this condition and there has never been a single case linked to vaping.
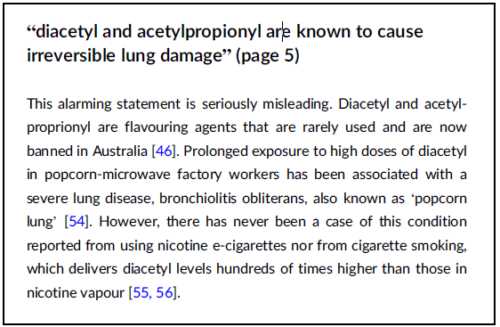
‘Popcorn lung’ (bronchiolitis obliterans) is a serious, but rare lung disease first detected in popcorn factory workers. It was linked to very high levels of ‘diacetyl’ which is used to create a buttery flavour.
Some earlier e-liquids contained diacetyl, however the levels found in vapour were hundreds of times lower than in cigarette smoke and there has never been a case of bronchiolitis obliterans due to smoking or vaping. Diacetyl is now rarely used and is banned in Australia in e-liquids.
According to leading health organisations
- Health Canada: “Vaping is not known to cause Popcorn lung”
- Cancer Research UK: “E-cigarettes don’t cause the lung condition known as popcorn lung. There have been no confirmed cases of popcorn lung reported in people who use e-cigarettes”
- Public Health England: Vaping does not cause popcorn lung
- UK National Health Service. “Vaping does not cause ‘popcorn lung’, the common name for a rare disease called bronchiolitis obliterans”
However Australia’s peak health and medical research body, the NHMRC falsely claims that vaping causes popcorn lung in its 2020 CEO statement on vaping and has refused to withdraw this claim, in spite of being advised of the evidence in our review in Addiction:
Reading: Minton M. Debunking the myth that vaping causes popcorn lung. Reason Foundation 2023
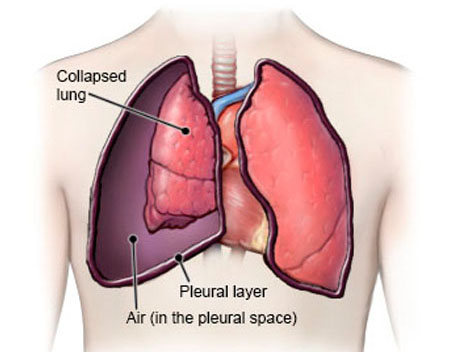
There is no evidence that vaping causes spontaneous pneumothorax.
A spontaneous pneumothorax is the sudden collapse of a lung without any apparent cause. It occurs when a congenital bleb or ‘bulla’ on the surface of the lung ruptures. Air is released from the lung into the chest cavity (pleural space) and the lung collapses.
Spontaneous pneumothorax occurs mainly in healthy young people without underlying lung disease, and can be sometimes triggered by smoking, strenuous exercise e.g., heavy lifting or severe coughing. It is most common in the 15-34-year-age group, especially in tall, thin young men. About 90% of cases in this age group are spontaneous. ‘Spontaneous’ means there is no underlying cause.
“Secondary” pneumothorax is caused by underlying lung disease. The most common cause is emphysema but also pneumonia, lung cancers, asthma, pulmonary fibrosis, and cystic fibrosis. Secondary pneumothorax is less common and occurs mainly in older people (55+).
Pneumothorax is common. For example, in England it occurs in 24 men and 10 women out of every 100,000 people each year. In fact, I personally was admitted to hospital with a spontaneous pneumothorax at the age of 20, and neither smoked or vaped.
In Australia, with 1.6 million adult vapers, most being under 40, there would be over 200 cases of spontaneous pneumothorax each year in young people who vape. This is based on 17 cases per 100,000 people per year, of which 90% are spontaneous.
The occurrence of vaping and this condition is an association. There is absolutely no reason to suggest that vaping causes spontaneous pneumothorax.

There is currently no definitive evidence that vaping increases the risk of cardiovascular harm. Long-term epidemiological studies are needed to provide more conclusive answers.
However, the potential harm is likely to be small in most cases and significantly less than that caused by cigarette smoking. The risk is greatest in heavy or long-term vapers and those with pre-existing cardiovascular conditions.
In contrast, the evidence is clear that switching from smoking to vaping substantially reduces the risk of cardiovascular disease
The evidence
1 Cross-sectional studies
Cross-sectional studies provide a snapshot of a population at a single point in time. While they can identify associations between vaping and health outcomes, they cannot determine whether vaping caused those outcomes.
Some cross-sectional studies have reported an association between vaping and a higher risk of cardiovascular issues compared to non-vapers. (Sharma; Alzaharani; Farfan; Vindyal) However, in many instances, participants who vaped had a history of smoking, and the increased harm may be attributed to their previous smoking habits. In some studies, cardiovascular events occurred before the onset of vaping.
Other cross-sectional studies have not identified any increased risk. One study of 450,000 subjects found that people who vaped but had never smoked had no increased risk. (Osei) Another study of 60,000 subjects found no increased incidence of heart disease in vapers compared to non-vapers. (Farsalinos)
2. Longitudinal studies
Longitudinal studies follow subjects over time. They are more robust and provide more reliable information.
A study of 24,000 subjects found that vapers who had never smoked had the same risk as non-vapers after five years follow-up. (Berlowitz) Another study found that vapers did not have an increased incidence of heart attack or stroke compared to non-vapers and non-smokers after five years. (Hirschtstick)
3. Cross-sectional and longitudinal studies
An analysis of 20 studies (14 cross-sectional and 6 longitudinal) involving nearly 9 million people did not find an increased incidence of cardiovascular disease in people who exclusively vaped compared to those who had never vaped or smoked. (Chen) The authors point out that this study does not prove that vaping is risk-free to the cardiovascular system – longer studies may be needed to identify harms.
4. Dual use
Numerous studies have found that dual use (smoking and vaping) significantly increases the risk of cardiovascular disease. (Chen; Berlowitz)
Does switching to vaping improve heart health?
The harm to the cardiovascular system from smoking far outweighs any potential risks from vaping (Peruzzi; Ding; Sharma)
Switching from smoking to vaping has been shown to reduce cardiovascular risk. Research has documented improvements in cardiovascular health in the short term (Caruso), within one month (George), and also at three and six months. (Klonizakis)
Studies have demonstrated significant improvements in blood pressure control among smokers with hypertension who switch to vaping, with benefits observed at a 12-month follow-up. (Farsalinos; Polosa) Additionally, both heart rate and blood pressure tend to decrease after switching from smoking to vaping. (OHID p956, 963)
Biological Plausibility: How might vaping cause harm?
While most of the toxic chemicals found in cigarette smoke are absent from e-cigarette vapour, some toxicants are present which could impact cardiovascular health. These include acrolein, oxidizing chemicals, volatile organic compounds (such as acrolein and benzene), and trace metals. However, these substances are present at much lower levels in vapour than in smoke. (OHID)
Studies in cells, animals and humans have found that vapour can affect cardiovascular health in several ways, the most potent being oxidising stress (harm to blood vessels from free radicals). Other mechanisms of harm include inflammation, sympathetic activation (increased pulse rate and blood pressure), platelet activation (increased stickiness in platelets leading to blood clots), harm to blood fats and endothelial dysfunction (damage to the lining of the arteries).
The risk to to human health from these findings is possible but uncertain. (Benowitz) Importantly, these effects are less pronounced compared to those caused by smoking. (Middlekauff; Ikonomidis)
What about the effect of nicotine?
Nicotine has well-documented effects on the cardiovascular system and could pose a risk for people with existing cardiovascular conditions. (Benowitz) However, these risks are much lower than those associated with smoking.
Nicotine increases heart rate and blood pressure, makes the heart work harder, and constricts blood vessels. It can also trigger arrhythmia (irregular heartbeat), cause insulin resistance (leading to elevated blood glucose levels) and may result in lipid (blood fat) abnormalities. Additionally, nicotine might damage the lining of the arteries. (Benowitz)
However, in the short term, nicotine use appears to pose minimal risk. A review of 42 clinical trials using nicotine products for up to 12 weeks found no significant increase in cardiovascular events. (Kim)
Furthermore, long-term users of Swedish snus (a product that delivers high doses of nicotine) do not have higher rates of heart attack or stroke compared to non-users. (Hansson)
Conclusions
1️⃣ There is strong evidence that smokers who switch to exclusive vaping substantially reduce their risk of cardiovascular disease.
2️⃣ There is no good evidence that exclusive vaping increases cardiovascular disease, although longer studies are needed to confirm this. Nevertheless, it is best not to vape if you are not a smoker or former smoker.
3️⃣ Dual use (smoking and vaping) significantly increases cardiovascular risk.

Many studies have found that adolescents, young adults and adults with depression are more likely to try vaping. (Lechner; Saeed; Gorfinkel; Javed). However, despite claims by some anti-vaping advocates, there is no evidence that vaping causes depression.
In fact, nicotine relieves depression and many people vape nicotine to make themselves feel better (known as “self-medication”). Nicotine acts in the “reward centre” of the brain to release the hormone dopamine, which creates pleasure. It also releases other chemicals in the brain, relieving anxiety and improving mood.
Adolescents often report vaping for stress relief. In the 2021 Canadian Tobacco and Nicotine Survey, the most commonly reported reason for vaping was to relax and relieve tension. A report by the NSW Office of the Advocate for Children and Young People in 2023 found that many young people use vaping as a coping mechanism “to manage their distress”. Vaping helped them deal with stress from home and school.
Higher levels of depression are associated with a faster escalation of e-cigarette use.
The beneficial effects of nicotine also partly explain why smoking rates are much higher in people with anxiety disorders and depression. However, smoking is deadly and smoking does far more harm overall than good.
One downside is that vapers who become dependent on nicotine can develop withdrawal symptoms when they cease vaping. These symptoms can include anxiety, loss of concentration, low mood and insomnia. In most cases these symptoms resolve over a couple of weeks. They are short-term and can be unpleasant, but are not harmful or serious.

It is best not to vape or smoke in pregnancy, however vaping is certain to be safer than smoking for the mother and foetus and is an effective quitting aid in pregnancy.
Safety in pregnancy
Unlike smoking, studies of vaping in pregnancy (here, here, here and here) have found little or no effect on birthweight, nor any increase in the risk of adverse birth outcomes.
A large randomised trial of 1,140 pregnant smokers by Hajek found that the safety of vaping was similar to nicotine patches and women who vaped were less likely to have babies with low birthweight (<2,500g). A recent re-analysis of this trial by Pesola found that pregnant women prefer vaping to NRT and “high quality evidence” that vaping “does not appear to be associated with any adverse outcomes“. The study also found
- Vapers have pregnancy outcomes similar to non-smokers
- Vapers had less cough and phlegm than NRT users
- The safety of vaping did not differ from using NRT
Women who smoke who switch to vaping in pregnancy should aim to stop smoking completely for the best results.
Nicotine replacement products such as patches, gums and lozenges are approved for use in pregnancy in Australia. Human studies here and here have not shown any clear harms from their use, such as stillbirth, premature birth, low birthweight, admissions to neonatal intensive care, caesarean section, congenital abnormalities or neonatal death.
Very high and chronic use of nicotine has been linked to harmful effects on the foetus in animal studies. However, there is no evidence that these findings apply to humans. Nicotine may not be completely safe for the pregnant mother and foetus, but it is always safer than smoking.
Quitting smoking
Although it is not risk-free, vaping has a role as a substitute for pregnant women who are unable to quit smoking with other methods. It should not be used by women who do not smoke.
A randomised controlled trial of 1,140 pregnant smokers found that vaping was twice as effective for quitting as nicotine patches (6.8% vs 3.6%). A cohort study of 1,329 pregnant women found that women who vaped were more than twice as likely as other those using NRT to report abstinence late in pregnancy (50.8% vs 19.4%). Vaping may also help to prevent relapse to smoking after birth.
Breastfeeding
Women who vape are more likely to breastfeed than women who smoke and also continue breastfeeding longer.
UK recommendations
The use of vaping in pregnancy is endorsed by an important expert group in the UK, the Smoking in Pregnancy Challenge Group, a partnership between the Royal College of Midwives, the Royal College of Obstetricians and Gynaecologists and the Royal College of Paediatrics and Child Health.
The Challenge Group provides the following advice to midwives:
“Very little research exists regarding the safety of using e-cigarettes (vaping) during pregnancy, however evidence from adult smokers in general suggests that they are likely to be significantly less harmful to a pregnant woman and her baby than continuing to smoke.”

Advice from the Challenge Group
The UK Royal College of Midwives 2019 Position Statement on quitting in pregnancy states:
“E-cigarettes contain some toxins, but at far lower levels than found in tobacco smoke. If a pregnant woman who has been smoking chooses to use an e-cigarette (vaping) and it helps her to quit smoking and stay smokefree, she should be supported to do so.”
The UK National Centre for Smoking Cessation and Training says, “if a person who is pregnant chooses to use a vape, and if that helps them to quit smoking and stay smokefree, they should be supported to do so.”
Reading
1. Use of electronic cigarettes before, during and after pregnancy. A guide for maternity and other healthcare professionals. Smoking in Pregnancy Challenge Group 2020
2. Position Statement. Support to Quit Smoking in Pregnancy. The Royal College of Midwives. 2019

Vaping is significantly less addictive than smoking. Smokers who switch to vaping find it easier to quit vaping (than smoking) when they are ready to try. [Shiffman 2020; Foulds 2015; Fagerstrom 2018; Hughes 2019; Liu 2018; Shiffman 2024)
Almost all former smokers who vape were already dependent on nicotine from past smoking but have transferred their nicotine dependence to a much safer product.
A comprehensive report commissioned by the UK Government in 2022 concluded that:
“the risk and severity of [nicotine dependence from vaping] is lower than for cigarette smoking”
“More addictive than heroin?”
It is wrong to say “nicotine is more addictive than heroin”. The dependence-forming characteristics of nicotine depend on how it is delivered i.e., how fast it reaches the brain and whether there are other chemicals that increase its effect.
- Smoking is particularly addictive because it delivers high levels of nicotine very rapidly to the brain. A review of 30 studies of nicotine delivery from vapes found that they deliver nicotine as quickly as smoking but to lower levels, and are therefore likely to be less addictive. (Cao 2024) However, some vaping devices can deliver nicotine as fast as smoking. (Nardone 2019)
- Smoke also contains other chemicals that make nicotine more addictive eg monoamine oxidase inhibitors. These chemicals are not present in vapour.
That is why dependence on nicotine patches is very uncommon. Less than 2% of patch users continue long-term.
A word on the definition of ‘addiction’
The urge to vape is not strictly characterised as “addiction”. According to Addiction Ontology, the definition of addiction is a compulsion to engage in a behaviour known to cause serious net harm.
Nicotine has only minor health effects and the urge to vape is best described as dependence. Dependence means having the urge to use a drug to avoid physical symptoms of withdrawal when it is ceased.
Many people do not regard dependence on nicotine from vaping as a problem as it provides many beneficial and enjoyable effects.

Switching from smoking to vaping is simply changing the source of nicotine from a deadly delivery system (a cigarette) to a far less harmful, potentially lifesaving alternative.
With vaping, there is no burning and therefore no tar, carbon monoxide and other harmful constituents that are inhaled from tobacco smoke. Vaper is a far safer and less addictive source of nicotine.
Some former smokers continue vaping long-term to avoid relapse to smoking. However for many, vaping is a temporary transition stage and many go on to quit vaping as well as smoking.

Wrong. Even frequent vaping is far safer than smoking and each puff is far less harmful.
Smokers and vapers puff to get the right level of nicotine their brain needs. A cigarette has to be consumed in one sitting, usually in 10-12 puffs, to deliver the nicotine hit. Vapers often ‘graze’, i.e., regularly take a few puffs on their vape as needed to maintain their nicotine levels through the day.
Vapers generally get less nicotine than smokers and it is usually delivered more slowly. More importantly, the nicotine is not accompanied by the thousands of toxic chemicals in smoke from burning tobacco.
You should use your vape as often as you need to get sufficient nicotine to prevent cravings and avoid relapse to smoking.

“Exposure” by children to nicotine vapes is often reported in the media, but poisoning and serious harm are rare. Accidental ingestion of nicotine is usually followed by intense vomiting and most cases resolve without treatment.
Accidental poisoning from nicotine e-liquid is especially rare when compared to poisoning from other chemicals and medicines. However, if a child swallows nicotine e-liquid, medical advice should be sought immediately.
Poisons Information Centres document ‘exposures’ to nicotine e-liquid which are often incorrectly reported by the media as ‘poisoning’. However, the Australian government says “Poisoning occurs when someone is sufficiently exposed to a substance that can cause illness, injury or death”.
‘Exposures’ are simply phone calls about actual or potential exposure or a request for information. Calls could include an enquiry from a worried parent that a child had touched a vape or put a vape in the mouth.
In 2022, the NSW Poisons Information Centre (PIC) received 213 calls about ‘exposure’ to nicotine e-liquid by children under the age of four. No serious outcomes were reported in the media. In comparison there were 927 calls about hand sanitiser, 834 calls about dishwasher detergent and 788 calls about toiler cleaner in this age group.
The Victorian Poisons Information Centre reported low rates of exposure to liquid nicotine in 2018 and 2019. The number of cases referred for treatment was 14 in 2018 and 15 in 2019. The claim by the Health Minister (19 June 2020) that nicotine poisoning had doubled during this time period is incorrect.
There has been one death in Australia from accidental nicotine liquid poisoning. In May 2018, an 18-month old child died after drinking from an open (non-childproof) bottle of imported concentrated nicotine (100mg/mL) when the mother was mixing the nicotine with locally purchased flavours. This tragic case underlines the importance of allowing the sale of low-concentrations of nicotine liquid, so it is available in child-proof containers with warning labels.
Three other accidental child deaths have been reported globally since 2013: one each in Israel, Korea and the US.
Accidental nicotine poisoning is rare in other western countries such as the United States, United Kingdom and Canada. Most cases are mild and self-limiting.
According to a review by Public Health England, the risks of ingestion of e-liquids appear comparable to similar potentially poisonous household substances.
Any poisoning risk should be considered in the context of 21,000 annual deaths from smoking in Australia. Many of these could be prevented by the wider use of vaping nicotine.
Exposure to poisons is widespread in society and is associated with many products from which society benefits, such as bleach and laundry detergents. These are managed by common-sense, warning labels and child resistant containers – not by bans.
Rechargeable lithium ion batteries in vapes can malfunction (“thermal runaway”) resulting in thermal and chemical burns and traumatic injuries. These incidents get a lot of media attention, but fortunately are very rare and most can be prevented.
Malfunctions of this type do not occur in the popular beginner models, ie sealed pod devices and pen-style models in which the battery is built-in and not removable. These devices are regulated and have an integrated circuit (chipset) to maintain electrical safety and protect the device from overheating. It cuts out the power if there is a malfunction or if the fire button is pressed for too long.
Nearly all ‘exploding e-cigarette’ stories you hear about on the news aren’t from regulated, properly handled vaping products. They are mostly from loose spare batteries being carried around in a pocket or purse where they come into contact with metal objects like keys or coins and discharge accidentally.
‘Mechanical mods’ used by some experienced users they do not have built-in electrical protection and must be used with great care. Sometimes incidents also occur with devices which have been tampered with.
Lithium ion battery malfunctions also occur in other electrical devices such as mobile phones, laptops and electric cars.

Injuries from vapes are rare and are far less common than injuries from tobacco cigarettes. Cigarettes remain the biggest cause of fatal house fires. According to the London Fire Brigade “Switching from smoking tobacco to vaping can greatly reduce the risk of dying in a fire”.
Most incidents could be prevented by user education eg
- Plastic storage cases to avoid contact of loose batteries with keys or coins. Never carry a loose battery in your pocket or handbag

Plastic case for a 18650 battery
- Only use reputable battery brands from trusted suppliers
- Never buy recycled batteries, re-wrapped or reclaimed batteries
- Avoid “mechanical mods” which lack safety features
- Always use the supplied USB cable as the amp rating of the cable matches the specifications of your device. Connect the other end to a good quality low amp (0.5-1 amp) USB wall adapter. Check the manual for advice
- It is safe to plug the USB cable into a computer, TV or game console as they provide a low, steady electrical output
- Phone and tablet chargers are generally not suitable for charging vapes as almost all are rated ≥2 amps output and deliver too much current
- Use a dedicated battery charger for loose batteries
- Do not keep your device on charge for longer than necessary and never leave it unattended when charging. Charge the device on a nonflammable surface in case of overheating
- Replace or re-wrap batteries if the cover is damaged
- Dispose of used batteries in a recycling bin, not in the household rubbish
Reading
11 Battery Safety Tips to Keep You Protected, Vaping 360 July 2023
Quitting Smoking

Vaping nicotine is a more effective quitting aid than nicotine replacement therapy (patches, gums, lozenges) and is at least as effective as varenicline (Champix). Vaping has helped millions of smokers quit who were unable to quit with other methods.
Studies show that vaping is effective in the controlled setting of randomised controlled trials, in natural real-world studies and with or without support.
RANDOMISED CONTROLLED TRIALS
The best scientific evidence that a treatment works is from randomised controlled trials (RCTs), in which subjects are randomly allocated the treatment (in this case vaping) or something else in a carefully controlled setting and the outcomes compared. The gold standard is Cochrane reviews which pool and analyse results (‘meta-analyse’) from the best RCTs to give even more reliable results.
RCTs underestimate the effectiveness of vaping. RCTs are limited to short time frames, typically 6 months. Real-world studies show that many smokers quit early but others switch successfully over time, some taking 2 years or more to adjust to vaping (eg Kim 2024). These quitters are not captured in RCT results. Also in RCTs, smokers cannot chose their preferred product and must use the device and flavour supplied.
1. Nicotine replacement therapies (patch, gum etc)
A Cochrane review in 2024 compared the effectiveness of vaping with NRT as a quitting aid with professional support and found “high certainty” evidence that vaping was 59% more effective than NRT.
Other meta-analyses of the best quality RCTs concluded that vaping was 53-77% more effective than nicotine replacement as a quitting aid. (eg Levett 2023; Grabovac 2021; RACGP 2021)
2. Varenicline (Champix)
Varenicline is the most effective conventional quitting aid but is used infrequently. One RCT compared varenicline directly with vaping and found that quit rates were equally effective after 6 months. (Tuisku 2024)
A 2023 Cochrane review found high-quality evidence that nicotine vapes and varenicline (Champix) are the two most effective single treatments for quitting smoking available in Australia. The study analysed 319 randomised controlled trials of all medications used to help smokers quit and found that for every 100 people who use vapes to quit, 10-19 are likely to succeed after 6 months or more. More here.
A review by the UK National Institute for Health Research analysed 363 RCTs of smoking treatments and concluded that vaping was the most effective single therapy, followed by varenicline and nicotine replacement therapy (NRT).
TRIANGULATION WITH OTHER RESEARCH
Combining different types of research with different strengths and weaknesses (triangulation) provides a more accurate picture than just RCTs alone. These studies all point to the same conclusion, strengthening the evidence that vaping is an effective quitting aid. They also show that vaping works in the real-world setting, not just in a controlled trial (RCT) setting.
1. Observational studies
Observational studies examine whether vaping works by observing its impact in a cohort of smokers in real-world settings. The findings are less reliable than RCTs but still give valuable information. The better quality observational studies show that vaping increases quitting (eg Goldenson 2021; Adriaens 2021; Kotz 2022).
2. Population studies
Multiple large population studies have found that smokers who vape to quit have significantly higher quit rates and quit success than smokers who do not vape, for example in the United States and in the United Kingdom. A study in Australia, Canada, England, United States found that smokers who initiated daily vaping were more likely to make a quit attempts and were three times more likely to have quit 12-24 months later. Non-daily vaping was not effective in increasing quit rates. Daily vapers are 3–8 times more likely to quit than smokers who do not vape.
An Australian population study by Chambers found that smokers who attempted to quit with vaping were twice as likely to have quit smoking for more than a month, 12 months later than those who did not try vaping (excluding those who vaped only once or twice). Higher quit rates are expected in a more supportive regulatory environment.
3. Declines in national smoking rates
Many western countries which provide legal access to vaping have experienced rapid declines in national smoking rates (see below). Vaping is not the only factor at play but is likely to be a major contributor.
4. England Stop-Smoking-Services
Analysis of quit attempts by the Stop Smoking Service in England shows that smokers have greater success in quitting by vaping with professional support compared to any other quitting method (64.9% vs 58.6%). (OHID 2022)
5. Accidental quitters
Vaping is unique as a quitting aid in that many smokers with no intention to quit, who try vaping, go on to quit without any support. Accidental quitters are surprisingly common and are not captured in RCTs. Studies include Kasza 2021; Foulds 2022; Carpenter 2023.
6. Anecdotes
Anecdotes are the weakest type of scientific evidence. However in 2021, there were an estimated 82 million vapers globally and many more had quit smoking and vaping completely. At these levels, anecdotes can’t be ignored.

Smoking rates are falling faster in countries which adopt vaping and other reduced risk nicotine products (such as snus and heated tobacco products) compared to countries that do not.
Vapes have the potential for a substantial positive public health impact (a function of reach × efficacy), given that vapes are both more effective and have a greater reach than other approved cessation methods. Vapes are the most popular quitting aid used in Australia and in most other Western countries.
In New Zealand from 2016-2023 daily smoking declined by 53.1% from 14.5% in 2016 to 6.8% in 2023 as vaping rates increased. In Australia, during the same period, daily smoking declined 32% from 12.2% in 2016 to 8.3% in 2023. Some of this decline is likely to be due to the uptake of illicit NVPs.
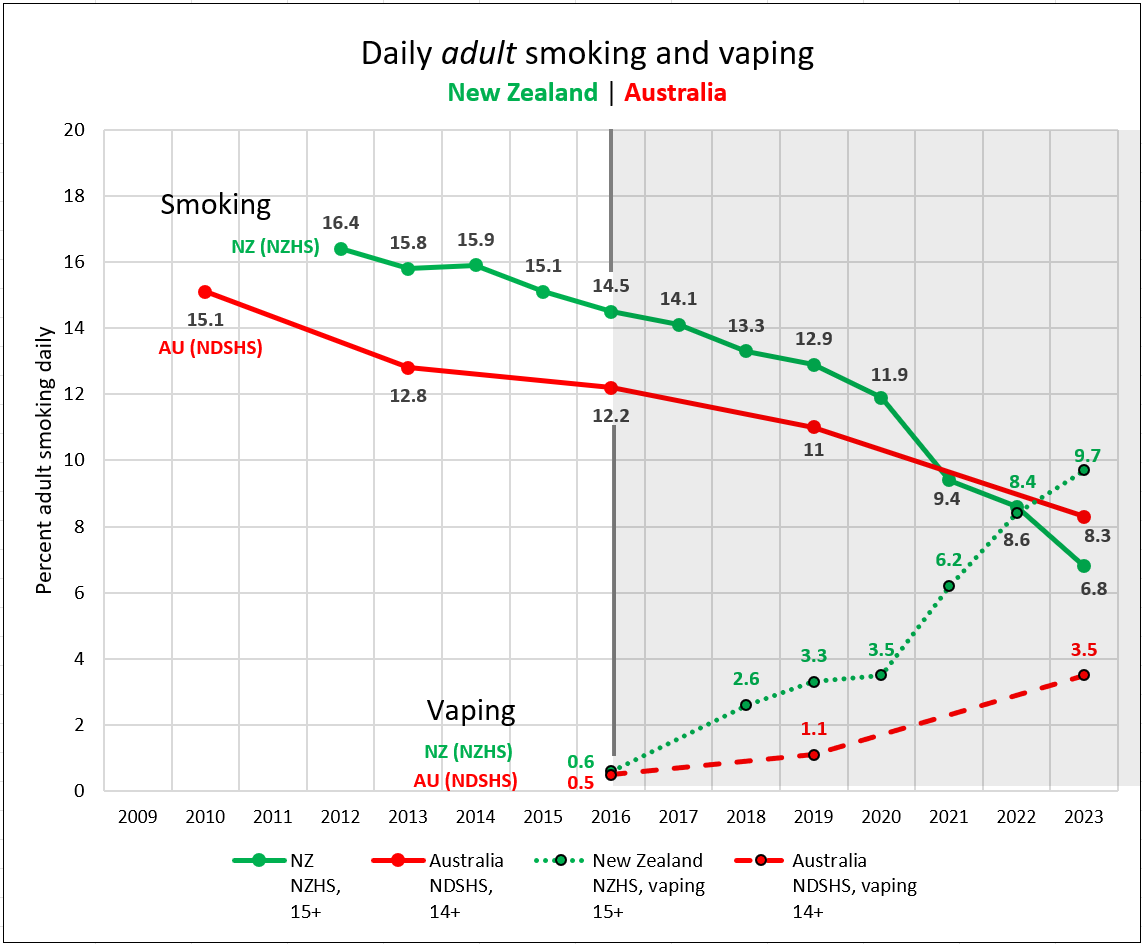
Decline in smoking in New Zealand accelerated as vaping increased
Smoking declined most in the age groups with the highest vaping rates, suggesting that vaping is a significant contributing factor (NDSHS 2023). Vapes help smokers quit and divert would-be smokers away from the deadly habit.
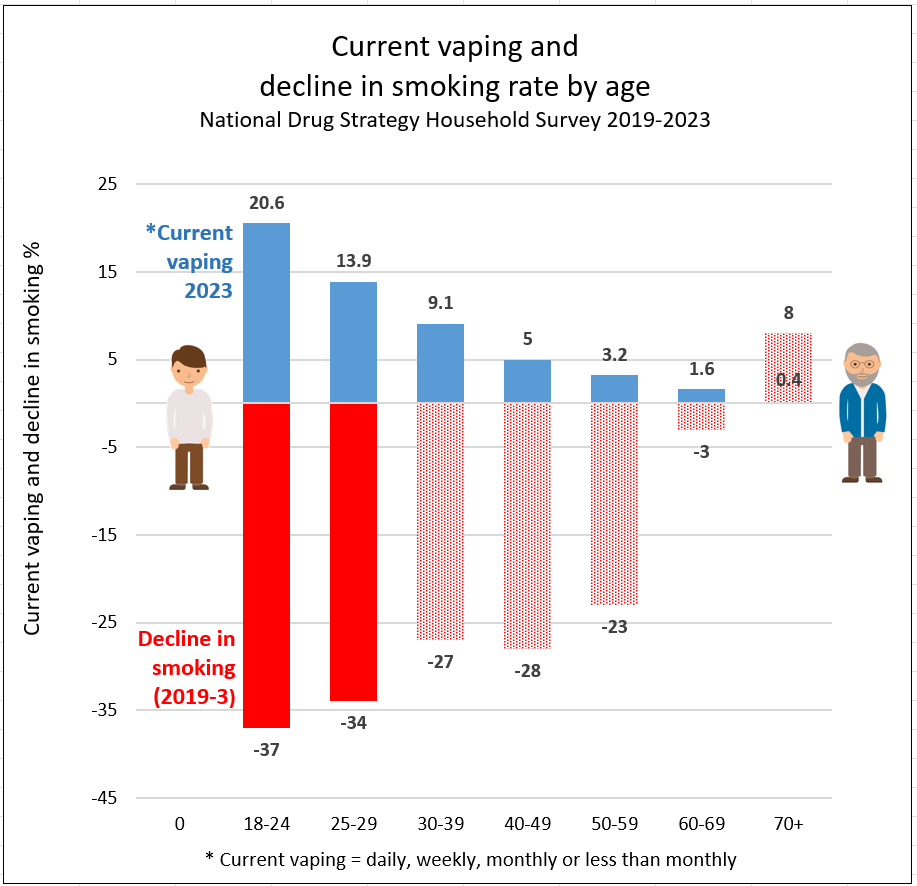
Decline is smoking 2019-2023 is fastest in the age groups with the highest vaping rates
Studies show that vapes function as economic substitutes for cigarettes. For instance, higher cigarette prices are associated with lower cigarette purchases but higher vaping purchases. Likewise, there is some evidence that higher e-cigarette prices are associated with higher cigarette purchases.
There is evidence that restrictions imposed on vape sales has the harmful unintended effect of driving tobacco users back to cigarettes, which are far more harmful to health.

Vaping nicotine is the most popular quitting aid in Australia and in many countries where it is readily available.
In 2023, 32% of Australian smokers used vaping to help them quit (19.6%) or reduce (12.2%) smoking. The next most popular quitting aid was nicotine replacement therapy (17%).
Vaping devices are also the most popular quitting aid in England, the United States and the European Union. Vaping devices were used in 43% of quit attempts In England in 2024 and in 27% of quit attempts in France.
Because of its combined popularity and effectiveness, the public health impact of vaping is even greater. Vapes even have a wider reach as they can assist those who are not planning to quit (accidental quitters), unlike conventional medicines.
Only short-term use is recommended but long-term vaping is safer than relapsing to smoking.
It is recommended that smokers should try to stop vaping once they have successfully quit smoking. However, for many former smokers, relapse to smoking is a constant risk. Research suggests that vaping may assist in preventing relapse. Vaping can act as a substitute for smoking behaviour to help cope with urges to smoke.
Smokers vary in the length of time they continue to vape after switching from smoking. The number vaping gradually declines over time, although some vapers need to vape long-term to prevent relapse to smoking.
How long do people vape?
About 70-80% of smokers who quit with vaping are still vaping 6-12 months later:
- An analysis of 19 randomised controlled trials: 70% of those who had successfully quit were still vaping at 6 months or longer (Butler 2022)
- A US cohort study of 2,535 smokers: 72% were still vaping 12 months later (Chen 2020)
- An RCT of 886 patients in England: 80% were still vaping at 12 months (Hajek 2019)
- In a cohort study of smokers who purchased a Juul device, 87% of quitters were still vaping at 24 months (Kim 2024)
In Great Britain, 55% of current vapers had been vaping for over 3 years, according to the annual ASH UK report in 2023. ASH UK also reported in 2024 that, among all ex-smokers who have ever vaped (including current and ex-vapers) the median length of time spent vaping was two years.
Of course, many former smokers who quit with vaping are now neither smoking or vaping.
Remember, “abstinence from nicotine is not necessarily a priority, the most urgent priority is to switch away from smoking tobacco”. (UK NCSCT)

There is no evidence that vaping causes former smokers to relapse, as claimed by some researchers (Baenziger).
Some studies have found that former smokers who later take up vaping are more likely to relapse than those who do not take up vaping. However, this association is not causal (caused by) vaping. There are two likely explanations for this finding:
- Former smokers who are tempted to relapse are more likely to try vaping to prevent going back to smoking. (Dai; McMillan) However, these smokers are already at risk of relapse. The relapse is not caused by vaping.
- Smokers who vape are more nicotine dependent than smokers who do not vape and are therefore more likely to relapse anyway, not because they vaped. (McNeill; Farsalinos)
Other research suggests that vaping is likely to reduce the risk of relapse. “Ex-smokers experience vaping as a pleasurable and enjoyable direct substitution for smoking” and this may be protective against a smoking lapse. (Notley 2018, Notley 2019)

You should only try to quit vaping when you are confident that you will not relapse to smoking as the small health risk from continuing to vape is minor compared to the harm from relapsing to smoking.
Quitting vaping is generally much easier than quitting smoking as vaping is less addictive. Some people can stop vaping abruptly, using techniques to manage urges, such as distraction and a commitment to the ‘not-a-puff’ rule.
1. Reducing nicotine and vaping frequency
You can gradually reduce the nicotine content of your vape and try to use it less frequently. Reducing nicotine levels may require an “open” vape system so you can fine tune your dose reductions. You may wish to vape nicotine-free e-liquid for a while before quitting.
You can also gradually increase the time between vaping sessions and set rules for when and where you do and do not vape to gradually reduce use. Try limiting vaping to certain places, times or situations.
2. Behavioural strategies
Behavioural strategies that are used to quit smoking may help. These include
- Distraction. Distract yourself when you get a craving by doing something else. Go for a walk, do some deep breathing, do some chores
- Avoidance. Some triggers can be really hard to deal with, such as vaping while drinking or vaping with friends. It may be best to avoid those situations for 2-3 weeks until you feel stronger.
- Delay. Cravings only last 2-3 minutes on average, although they feel like a lot longer! If you can delay the thought of vaping for 10 minutes, for example, until a certain time or after completion of a task, the craving will almost invariably be gone.
- Escape. If the pressure is mounting and you think you are going to crack, just leave! Go home, go for a walk, just get out of there!
3. Lifestyle changes
Other lifestyle changes can help, such as keeping busy, doing regular exercise, relaxation strategies and drinking less alcohol.
4. Medication
Some people benefit from switching to nicotine replacement therapy, such as patches or gums, as a step to quitting. There is some evidence that a course of varenicline tablets (Champix) can also help you stop vaping. This needs to be prescribed by your doctor.
However if there is any risk of relapse to smoking you should continue vaping.
After quitting, it is a good idea to keep a vape or faster-acting NRT (eg gum or lozenge) at hand for ‘emergency’ situations when a sudden trigger causes an urge to smoke.
Further information
Supporting clients who want to stop vaping. National Centre for Smoking Cessation and Training, UK. 2022
Wahhab M. Clinicians guide to supporting adolescents and young adults quit vapes. Sydney Childrens Hospital Network 2023
A Guide to Support Rangatahi (children) to Quit Vaping. NZ Asthma and Resp Foundation 2023
Youth vaping

About five percent of young people in Australia who have never-smoked vape frequently. Most youth vaping is experimental and short-term. This is a far cry from the alarmist media headlines of a youth vaping ‘epidemic’.
From a health point of view, the main concern is for never-smoking teens who vape frequently as this is the group at risk from new and potentially harmful inhaled chemicals. However, frequent vaping is mostly by adolescents who are or have been (or would be) smokers. Vaping for this population is likely to be beneficial.
Media reports usually refer to lifetime (ever-vaping) or past-12 month vaping. These measures exaggerate the risk as most teen vaping is experimental and short term, especially by never-smokers.
The research
The Australian Secondary Students’ Alcohol and Drug Survey (ASSAD) in 2023 surveyed nearly 10,000 12-17-year-old secondary school students. Of these 29.9% had ever tried vaping and 15.7% vaped in the last month.
Only 4.8% vaped ≥20 days in the last month and 3% vaped daily. 31% of vapers had already tried smoking or currently smoked, so overall around 5% of never-smoker were frequent vapers.
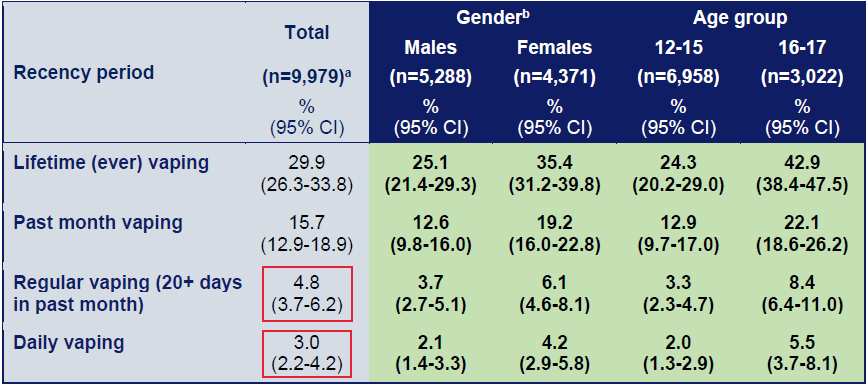
Vaping by age and gender in secondary school students 2022-23 (ASSAD)
The National Drug Strategy Household Survey in 2023 surveyed 560 14-17-year-olds. Of these, 28.4% had tried vaping. However half of these (14.2%) had only vaped once or twice.
Only 3.5% vaped daily and an estimated 3% vaped 20+ days per month, but not daily (6.5% total). Some were smokers who switched to vaping (21% had smoked first). So an estimated 5% of never-smokers vaped frequently (80% of 6.5%). Some of these young vapers would have become smokers if vaping was not available.
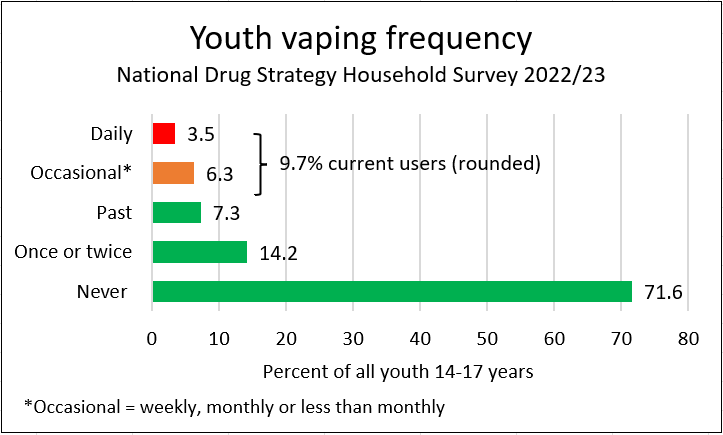
Youth vaping frequency (NDSHS 2023)
Other countries
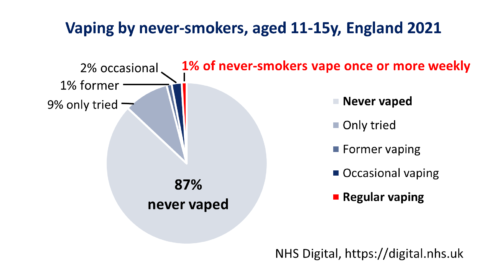
Frequent vaping by young never smokers is generally <2% in other western countries. (reference)
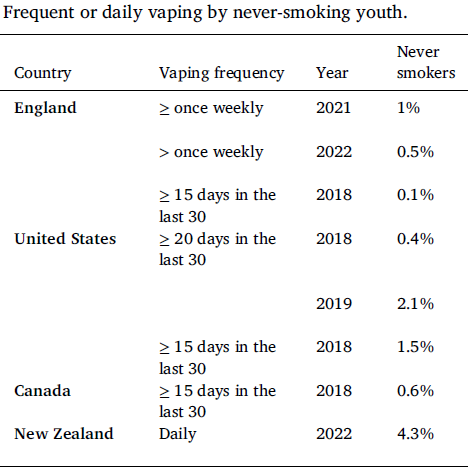
For example, in England in 2021, 7% of youth aged 11-15 years were currently vaping. [NHS Digital] However only 3% of never-smokers currently vape (1% at least weekly, 2% less than weekly).
Further reading
Mendelsohn CP, Hall W. What are the harms of vaping in young people who have never smoked? Int J Drug Policy 2023
Blog post. Frequent vaping by teen non-smokers is very uncommon in Australia, August 2023
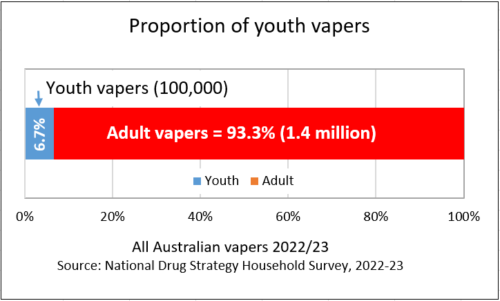
Only 6.7% of Australians who vape are youth aged 14-17 years, according to the 2022/23 National Drug Strategy Household Survey.
There are 100,000 14-17-year-old current vapers out of a total of 1.5 million current vapers aged 14+, see Table 3.4 (there would be an additional small number of 12-13-year-olds vaping who are not included in the NDSHS). The remaining 93.3% of vapers are adults aged 18 and over, most of whom have used vaping to quit smoking and are continuing to vape to avoid relapse.
In Great Britain, underage vapers (11-17 years) are estimated to be around 8% of the total vaping population.
This is still only a tiny fraction of the total vaping population.
However, government policy is disproportionately focussed on the small harms of vaping to this small minority. In doing so, it ignores adult welfare, interactions between adult and adolescent welfare and benefits to youth:
- Measures taken to prevent trivial risks to young people may create lethal consequences for millions of adults. Youth vaping presents a far lower and usually transient public health risk compared to the risks facing adults who have already smoked for years or decades.
- Young people do not live in isolation from adults and they benefit when adult smokers switch to vaping. The primary driver of youth smoking initiation is the smoking behaviour of parents or significant adults. Young people are also harmed by the economic and health impacts of parental smoking and from second-hand smoke exposure.
- Vaping is a relatively innocuous behaviour in young people compared to, say, binge drinking, driving under the influence, or illicit drugs.
- Also, vaping is beneficial to young people in that it diverts young people away from smoking overall.

Yes. The youth vaping rate in Australia is higher than in most other countries where vaping is regulated as an adult consumer product. Australia’s harsh vape restrictions are intended to reduce youth vaping but are having the opposite effect.
A review of current youth vaping rates in nearly 50 countries is summarised in the following graph (vaping in orange):
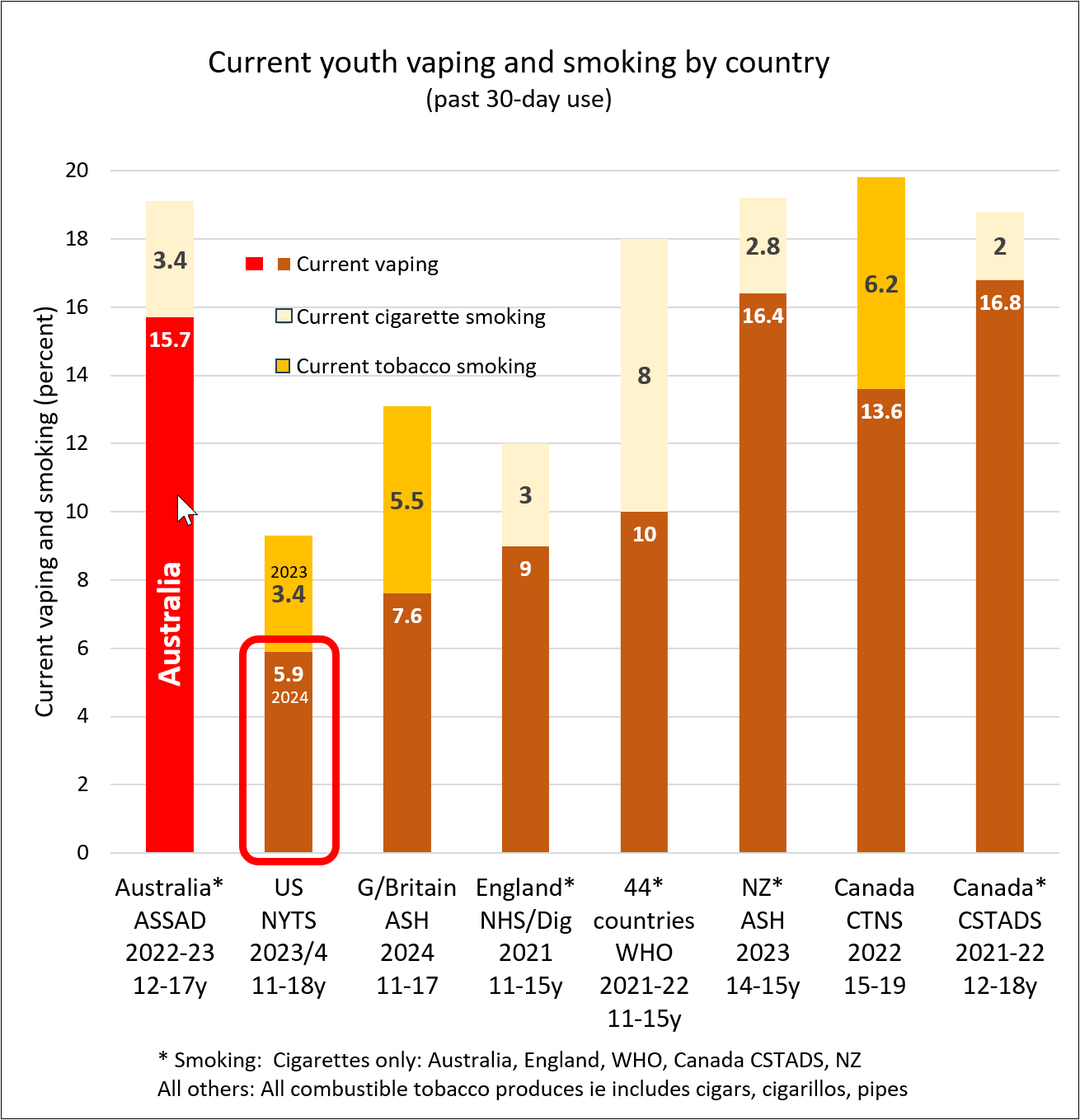
This graph shows nicotine use by young people in various countries.
See below for study details.*
If Australia switched from prescription-only regulations to an adult consumer model, it would make legal vapes more readily available for adults and reduce the black market which is supplying young people.
International trends
Youth vaping continues to rise sharply in Australia.
In contrast, youth vaping is declining in the US, Canada and New Zealand and has plateaued in Great Britain.
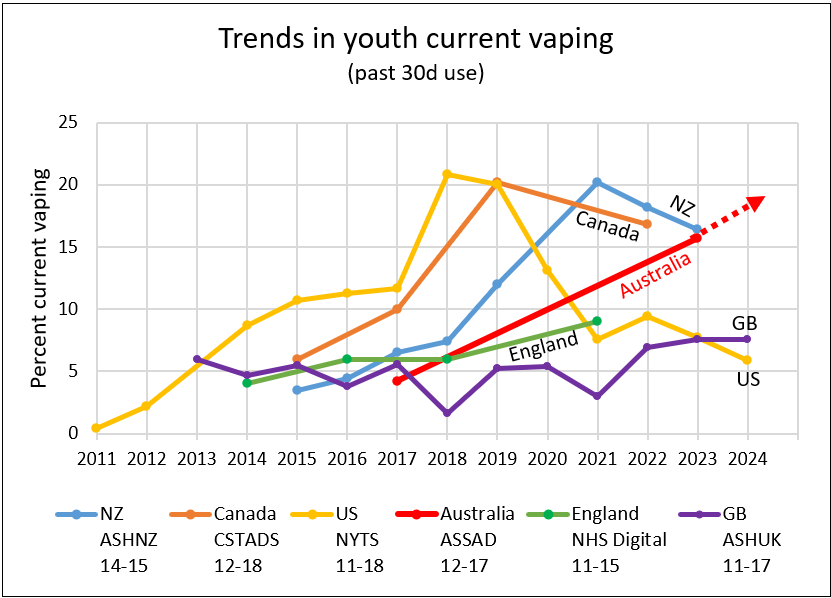
- In the US, vaping by middle and high schoolers (grades 6-12) declined by 70% in 5 years, from 20% in 2019 to 5.9% in 2024
- In Canada, youth vaping declined by 15.8% from 20.2% in 2019 to 16.8% in 2022
- In New Zealand, regular youth vaping declined by 19%, from 20.2% in 2021 to 16.4% in 2023
- In Great Britain, current youth vaping is plateauing over 2023-24
- In England, current youth vaping rose marginally from 6% in 2016 to 7% in 2021
Implications for policy
Australia’s de facto prohibition of vaping is driven by a moral panic about youth vaping but has not been effective in restricting youth uptake
The harsh restrictions have also created a range of serious unintended consequences
- Black market. They have also created a world leading rampant black market which supplies about 90% of users with unregulated products. In comparison, New Zealand (Submission 106) has no significant black market. In the UK, the black market is estimated to be around one third. In the US where the vast majority of products currently used have been banned by the FDA, an estimated half the market is illicit.
- Adult access. Access to vapes for adult smokers is severely restricted by requiring a doctor’s prescription and purchase from a limited range from pharmacies
- Lost taxation revenue. Billions of dollars of tax revenue and other economic benefits are unavailable from the current prescription-only model.
The benefit of legalising and regulating the sale of vapes as adult consumer products sold from licensed retail outlets has never been clearer. It would reduce youth vaping, give easier access to adult smokers, reduce the black market and generate government revenue.
Footnotes
* Studies included
The most recent and largest official youth surveys in Australia, the US, England, New Zealand and Canada:
- Australia: ASSAD, n=10,065 (2022-23)
- USA: NYTS, n=29,861 (2024)
- England: NHS Digital, n=9289
- Great Britain: ASH UK (details TBA)
- New Zealand: ASH Year 10 Survey, n=29,260
- Canada: CSTADS n=61,096
A large survey by the World Health Organisation published in April 2024 from 44 countries in Europe, Central Asia and Canada (data collection 2021-2022), n=279,117
- HBSC (WHO): Albania; Armenia; Austria; Belgium (Flemish); Belgium (French); Bulgaria; Canada; Croatia; Cyprus; Czechia; Denmark; Denmark (Greenland); Estonia; Finland; France; Greece; Hungary; Iceland; Ireland; Italy; Kazakhstan; Kyrgyzstan; Latvia; Lithuania; Luxembourg; Malta; Netherlands (Kingdom of the); North Macedonia; Norway, Poland; Portugal; Republic of Moldova; Romania; Serbia; Slovakia; Spain; Sweden; Switzerland; Tajikistan; United Kingdom (England); United Kingdom (Scotland); and United Kingdom (Wales).
Note that direct comparisons between the surveys can’t be made as they use different age ranges, definitions and are taken at different times.
Exclusions
These studies were not included due to small sample sizes:
- Australia: NDSHS 2022-23, n=560
- New Zealand: New Zealand Health Survey 2022-23, n=192

There is no good evidence that vaping is a gateway to youth smoking. Even if a gateway exists for some youth, it is far outweighed by the number of young people diverted away from smoking.
There are 5 strands of scientific evidence which undermine the “gateway theory”:
1. Common risk factors for vaping and smoking
Studies show that young people who experiment with vaping are three times more likely to also try smoking. However, there is no evidence that vaping causes them to take up regular smoking if they would not otherwise have done so. It is far more likely that there is a common liability to try a range of substances in adolescence. Young people who experiment with vaping are different to kids who don’t vape – they are more likely to use other drugs, have friends who vape or smoke, have mental illness, parents who smoke, come from lower socio-economic backgrounds, have lower education etc. These ‘shared risk factors’ put them at risk of experimenting with both vaping and smoking.
Studies that allow for these differences between groups have found that the increased risk of smoking in teens who vape (compared to teens who don’t vape) dramatically reduces or disappears. For example, Kim 2019, adjusted for 14 shared risk factors and concluded that:
“The apparent relationship between e-cigarette use and current conventional smoking is fully explained by shared risk factors, thus failing to support claims that e-cigarettes have a causal effect on concurrent conventional smoking among youth”
Other studies that account for a comprehensive range of shared risk factors have found the same thing, for example, Sun 2021 and Cheng 2020.
2. Accelerated decline in youth smoking
The gateway theory predicts that vaping will increase smoking rates in young people. However, we are seeing the opposite of this. In countries where vaping is readily available such as the UK, US and New Zealand, the decline in youth smoking rates has accelerated (Delnevo and Villanti 2021; Pesola 2021; Levy 2019; Meza 2021; NHS Digital UK 2022; ASH NZ 2022), suggesting there is no overall gateway effect.
For example, since vaping became popular in the US in 2013, smoking by high schoolers has fallen 10% faster than the previous decline.
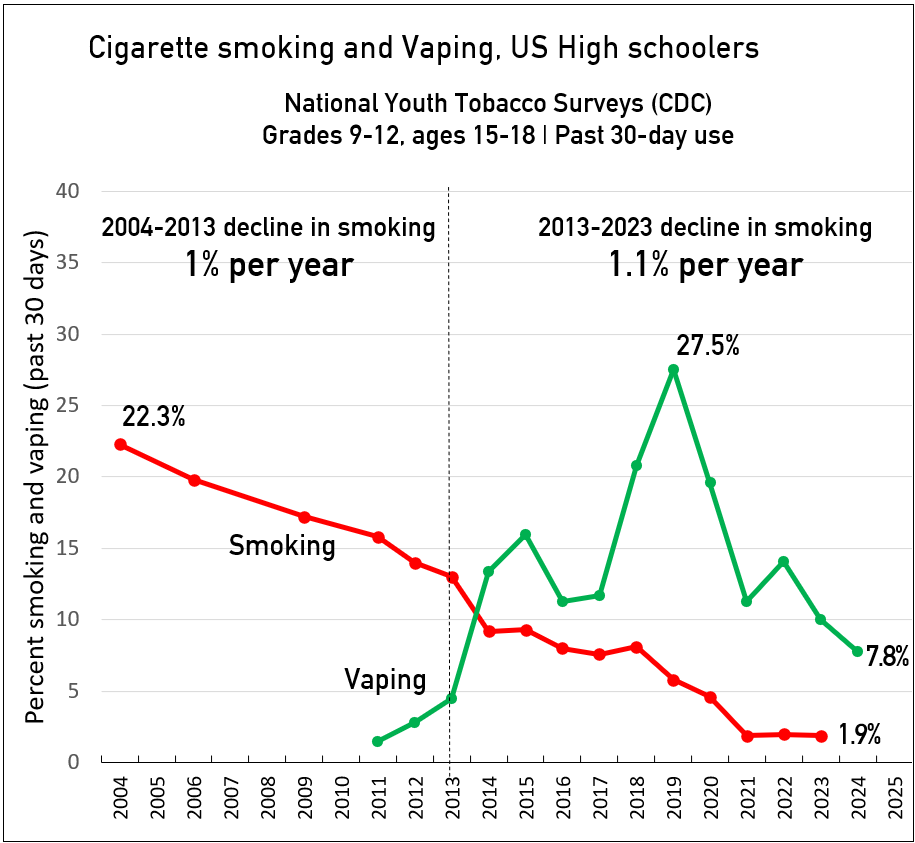
3. Vaping diverts young people from smoking
Many studies have found that vaping and smoking are substitutes and that vaping is diverting young people AWAY FROM smoking.
This has been demonstrated in modelling studies (Foxon 2020, Selya 2021, Sokol 2021) and in population studies (Walker 2020).
4. Restrictions on vaping increase smoking
Other research studies (natural experiments) have found that youth smoking rates increase when access to vaping is restricted. This has been demonstrated for
- Vaping bans (Friedman 2015)
- Increased prices of vapes (Cantrell 2020; Pesko 2022; Abouk 2023)
- Age of sale restrictions (Pesko 2016; Dave 2019; Pesko 2019; Pesko 2023)
These findings confirm that vapes and smokes are substitutes. Reducing access to vaping increases the uptake of deadly smoking.
5. Vaping first (before smoking) reduces smoking uptake
There is growing evidence that teens who vape first (before smoking) are less likely to smoke later, compared to those who smoke first (Shahab 2021; Legleye S 2021; Mus 2023) Other studies have found no evidence that vaping first increases smoking uptake (Chyderiotis 2020; Stanton 2023)
Reference
Summary of gateway studies referenced in this article, updated 2Oct2023
Selya A. Can the Theory of Youth Vaping as “Gateway” to Smoking Be Put to Bed? Filter2024Mendelsohn CP, Hall W. Does the gateway theory justify a ban on nicotine vaping in Australia? International Journal of Drug Policy 2020
Despite the flood of alarming stories in the media, vaping carries negligible health risk for young people who have never smoked if it doesn’t lead to long-term use.
This 5-minute video outlines the key issues:
Much of the concern about health effects is based on uncertainty or exaggeration, animal studies, correlation rather than causation and the effects of illicit products.
Most vaping by young non-smokers is infrequent and short-term, so they are exposed to low levels of chemicals and therefore low risk (not risk-free). A recent review of vaping by adolescents and young adults concluded
“Most e-cigarette usage is infrequent and unlikely to increase a person’s risk of negative health consequences”
Respiratory health
Symptoms
- Some studies have reported more respiratory symptoms in young people who vape than never-vapers e.g. cough, shortness of breath or wheeze (Brose 2024, Tackett) A review concluded that these respiratory symptoms tend to be transient and of uncertain significance. (Polosa)
- Other studies have concluded that there is no clear evidence that vaping causes “clinically significant” lung symptoms (Stevens and Tanski).
- A large US study of 12-17-year-olds found that vaping was not associated with respiratory symptoms, the onset of asthma or aggravation of asthma after 12 months (Yao).
Bronchitis, pneumonia, chronic cough
- A large US study of 12-17-year-olds found that exclusive vaping was associated with later reporting by parents of bronchitis, pneumonia or chronic cough (Zavala-Ariniega). This study does not prove that vaping caused these outcomes, but raises concerns.
Asthma
- The findings for asthma are mixed. Some longitudinal studies did not find an association between vaping and asthma (eg Mattingly, Patel, Yao) whereas two reviews did find an association (eg, Chand, Li). An association does not prove causation, but raises concerns.
Other lung conditions
- Vaping nicotine does NOT cause the serious lung disease E-cigarette or Vaping Associated Lung Injury (EVALI) or spontaneous pneumothorax (lung collapse) or ‘popcorn lung‘.
Brain development
High doses of nicotine can harm the adolescent brain in animal studies but there is no evidence of harm in humans. Even smoking has not been found to impair IQ, educational achievement or cognitive abilities later in life, so it is very unlikely that vaping will.
Other risks
There is no evidence that vaping nicotine causes seizures. There is a rare risk of burns and injuries from lithium-battery explosions, but none have been reported from disposables, the most popular type of device used by young people.
Nicotine dependence in never-smokers
Vaping can cause nicotine dependence in some young people who have never smoked. However, this is only in a small minority of cases. Nicotine withdrawal can cause short-term symptoms such as irritability, restlessness, anxiety, difficulty concentrating and depression. Nicotine otherwise causes little harm in the doses commonly used in vaping. Nicotine does not cause cancer or lung disease and it has only a minor role in cardiovascular disease.
In Australia, less than 2% of non-smoking 14-17-year-olds vape nicotine “frequently” enough to be at-risk of developing nicotine-dependence.
An analysis of the 2018 US National Youth Tobacco Survey found that <4% of young people who had vaped in the past 30 days but had never smoked had signs of nicotine dependence. This is to be expected as the dominant pattern of use is occasional and short-term.
Nicotine dependence is mostly concentrated in young people who have are past or current smokers.
Risk for former smokers
Vaping is not harmless, but is far less harmful than smoking. Young smokers who switch to vaping are likely to see health benefits.
Long-term risk
Adults who quit smoking by the age of 35 have a normal life expectancy (Doll). As vaping is around 95% less harmful than smoking, it is likely that youth who vape for several decades are highly likely to have only a minor effect on long-term harm.
The precise long-term effects of vaping nicotine will not be fully known for decades but are highly likely to be far less than from smoking. Ongoing monitoring and long-term studies are essential to detect any problems that may arise in the future, particularly from sustained frequent vaping.
References
Mendelsohn CP, Hall W. What are the harms of vaping in young people who have never smoked? International Journal of Drug Policy 2023
Mendelsohn CP, Wodak A, Hall W. How should nicotine vaping be regulated in Australia? Drug and Alcohol Review. April 2023. DOI: 10.1111/dar.13663
 Kids should not smoke or vape, but the benefits of vaping outweigh the risks at a population level. Rather than just focus on the harms of vaping, we need to do a formal risk-benefit analysis of youth vaping to assess its overall impact.
Kids should not smoke or vape, but the benefits of vaping outweigh the risks at a population level. Rather than just focus on the harms of vaping, we need to do a formal risk-benefit analysis of youth vaping to assess its overall impact.
The harms
The harms of vaping are summarised above. The key points are
- Frequent vaping by never-smokers is rare. About 1-2% of never-smoking teens vape regularly in western countries. Most use is occasional and short-term, so exposure to chemicals is very low in most cases.
- Nicotine dependence is rare in never-smokers as few vape frequently enough to get dependent. Nicotine dependence can be unpleasant, but is not serious.
- The harms to health are small. There is no evidence of ‘functionally important’ respiratory symptoms and vaping does not trigger asthma. Nicotine does not harm the adolescent human brain, nor does it cause EVALI, “popcorn lung” seizures or pneumothorax. Fires and explosions are very rare.
- Over the long-term, cardiovascular and lung effects may appear but these are highly likely to be small.
The benefits
- Rather than being a gateway to smoking, vaping is diverting some young people who would have smoked away from a lifetime of deadly smoking. As youth vaping increases, smoking rates are declining faster than ever in the UK, New Zealand and US.
- Some young smokers are switching from deadly smoking to much safer vaping.
- Vaping provides benefits such as pleasure, relief of anxiety and depression. Nicotine improves concentration and cognitive function, can help with weight control and improves ADHD and schizophrenia. Vaping helps some users socially.
Risk-benefit analysis
Vaping is not risk-free, but the benefits of youth vaping outweigh the modest risks at a population level, especially due to its impact in reducing smoking rates.
This is not to endorse youth vaping. Kids should not vape or smoke, but some kids will do one or both anyway. However, policy should not be driven by emotion or moral judgements. Evidence-based policy should consider the overall impact of vaping.
More here: Youth vaping: a risk-benefit analysis
Reading: Mendelsohn CP. It’s time to change the way we look at youth vaping. Filter Magazine, 14 July 2023
There is no evidence that nicotine causes harmful effects on the human adolescent brain.

Nicotine has been linked to harmful effects on the adolescent brain animal studies which mostly use chronic, high-dose exposure. However, given species and dosing differences, the extrapolation of these findings to humans is speculative. The rodent brain is not a reliable proxy for the human brain.
The UK Committee on Toxicity and an Australian review examined the evidence and concluded that no data were available on direct effects of nicotine exposure in human adolescents.
Also, there is no long-term evidence of impaired brain function in the hundreds of millions of adults who smoked as adolescents and then stopped.
Studies of young people who smoked have not found any difference in IQ, educational achievement or cognitive abilities in adulthood between those who have smoked in the past and quit and those who have never smoked. If adolescent smoking doesn’t lead to brain harm, it is highly unlikely that vaping will.
To put it bluntly, Professor Brad Rodu says: “Let me be crystal clear. The harm in brain development federal officials talk non-stop about only happens in laboratory torture of mice. There is absolutely no scientific evidence to support the claim that nicotine causes harm to human brain development.”
On the positive side, there is some evidence that nicotine may in the short-term improve attention, memory and cognitive function, relieve anxiety and improve mood.
Nicotine is especially beneficial for young people with ADHD, improving attention and brain function.
Nicotine in NRT is approved for use from the age of 12 in Australia, including in pregnancy.

Vaping is not “creating a new generation addicted to nicotine” as is often claimed.
Nicotine dependence from vaping is uncommon in young people who have never previously smoked. In Australian studies, about 3-8% of youth may have nicotine dependence. (NDSHS 2023; ASSAD 2023)
3-5.5% of youth based on self-reports
- ASSAD: 5.5% believed they would experience at least some difficulty going without vaping
- NDSHS: 3% report being “unable to stop or cut down”
7-8% based on frequent vaping
- ASSAD: 7.8% (4.8% vape 20days or more per month + 3% vape daily)
- NDSHS 7-8% (3.5% vape daily + estimated 3.5% frequent, but less than daily)
However some of these are former or current smokers. Some would be smokers if vaping was not available.
An analysis of the 2018 US National Youth Tobacco Survey found that <4% of young people who had vaped in the past 30 days but had never smoked had signs of nicotine dependence. This is to be expected as the dominant pattern of use is occasional and short-term.
A study by 15 past Presidents of the Society for Research on Nicotine and Tobacco concluded:
“Vaping likely addicts some young people to nicotine. However, the evidence does not suggest it is addicting very large numbers. Jarvis et al. concluded that “Data . . . do not provide support for claims of a new epidemic of nicotine addiction stemming from use of e-cigarettes.” Jackson et al. recently reported that the e-cigarette–driven increase in nicotine product use among high-school students is not associated with an increase in population-level dependence. Among tobacco-naïve youths, in addition to low vaping prevalence (9.1% in the past 30 days in 2020) and frequency (2.3% vaping ≥20 days in the past 30 days), small percentages exhibited signs of nicotine dependence.90
Frequent use is much more common among current or former smoking youths than among never-smokers. Many former smokers were already addicted to nicotine before initiating vaping. With high-school students’ smoking declining at an increasing rate since youths began using e-cigarettes, some may vape to reduce or quit smoking.”
Nicotine dependence is actually becoming less frequent. A study in the US youth showed that from 2010 to 2019 when vaping was it its peak, there was no increase in nicotine dependence overall, at least partly due to the shift from smoking to vaping (which causes less dependence).
Nicotine dependence is mostly concentrated in young people who are past or current smokers.
Is youth nicotine use increasing?
Australia’s National Drug Strategy Household Surveys show that daily nicotine use is only marginally raised and much lower than 20 years ago Importantly, daily youth smoking has almost been eliminated!
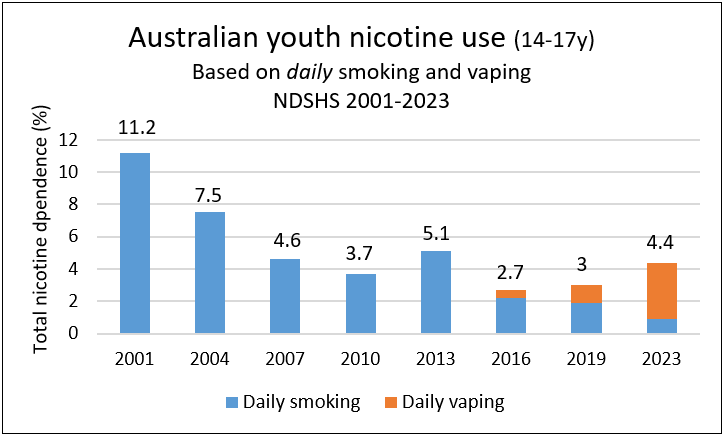

High levels of youth vaping are largely a result of failed regulations.
Under current Australian law, adult vapers are required to have a doctor’s prescription for nicotine to vape legally, but very few are willing to get one. This has created a thriving black market run by organised crime groups, which supplies dodgy, unregulated vapes freely to teens through rogue convenience stores and tobacconists or via social media.
Eliminating the black market is the key to reducing youth vaping. The only way to eliminate the black market is to replace it with a legal, regulated one.
A tightly regulated, risk-proportionate consumer model with strict age verification would make regulated vaping products more available for adults who smoke, reduce illicit sales and make vapes less accessible and less appealing to young people.
Measures to reduce youth access and appeal include
- Vaping products should be sold from licensed retail outlets where strict age verification is available such as vape shops and retail outlets where tobacco is sold. Sales to youth should result in severe fines and loss of licence.
- Flavour names that specifically appeal to young people such as ‘dragon vomit’ should be banned and only simple flavour ‘descriptors’ such as caramel or blueberry used.
- Packaging should be simple, without bright colours and images with youth appeal.
- Honest and accurate education to young people on the risks of vaping.
- Advertising should be carefully restricted and regulated to prevent appeal to adolescents.
- Online retailers should verify the age of the purchaser with a third-party age verification service.
- Verification of age on delivery.
- Clear public and youth education to frame vaping as a smoking cessation tool or a safer alternative for adult smokers. There should be a clear message that vaping is not for young people or non-smokers.
- Mandatory CCTV at point-of-sale to ensure compliance.
Further reading. Mendelsohn C, Wodak A, Hall W. How should nicotine vaping be regulated in Australia. Drug Alcohol Review 2023
Young adult vaping

It is highly likely that vaping is significantly reducing deadly smoking rates in this age group and may be beneficial overall to public health.
How many young adults vape?
In Australia, one in five (21%) 18-24-year-olds “currently” vape (ie vape once or more in the last 12 months). (NDSHS 2023) However, most vaping by young adults is infrequent and short-term, as the following graph shows.

Most vape only once or twice or have vaped in the past and quit. One in twelve (8.5%) vape daily. One in eight (12.7%) vape occasionally (once or more in the last 12 months).
Vaping is reducing smoking
It is highly likely that vaping is diverting young adults away from taking up smoking and is helping young adult smokers to quit
Data from the 2023 National Drug Strategy Household Survey show that the decline in smoking in the 18-24-year-old age group is faster than in any other adult age group.

Even if a small number of young adults are diverted from smoking there is likely to be a substantial public health benefit as smoking kills 2 in 3 long-term users.
This finding in Australia is consistent with international research. Many studies have confirmed that young adults have the highest vaping rate and the most rapid declines in smoking of all age groups. This has been demonstrated in populations in the US (Floxon; Sanford) and the UK. (APS; Tattan-Birch) This rapid decline in smoking became apparent only since vapes became more widely available.
The harm from young adult vaping
Even for daily vapers, the risks from vaping are low, especially for short-term use. The majority of those who try vaping do so temporarily, often only once or twice. These patterns of vaping carry no or minimal risk.
Smokers who quit before 35 years of age recover fully and have a normal life expectancy. (Jha 2014) It is highly likely that vaping for two or three decades will cause little harm as vaping carries only a small fraction of the risk of smoking. (OHID 2022)
Furthermore, smokers who have switched to vaping are likely to have substantial health benefits.
Importantly, there is no good evidence that vaping is a gateway to smoking. (more about the gateway here)
An adult choice
Remember we are talking about adults who are entitled to make their own informed choices. Nanny state activists and governments have no right to interfere with these choices as long as they are harming no-one else.
Australia’s paternalistic approach to vaping nicotine is in conflict with the Harm Principle, developed by the highly respected English philosopher John Stuart Mill in 1859.
Mill states that in a liberal democracy, adults of sound mind should have the freedom and autonomy to make their own lifestyle choices as they know best what is right for themselves whereas governments are often wrong
Vaping opponents apply a double standard to vaping and try to restrict it. However, young adults are legally able to smoke, drink, drive cars, bungee jump and parachute, all of which are far more harmful.
Other issues

Vaping is a quitting tool for smokers, however some non-smokers take up vaping. For some, this will be an alternative to smoking and is far less harmful.
In the 2022-23 National Drug Strategy Household Survey 3.5% of Australian adults (14+) who had never smoked vaped daily and a further 2.2% vaped weekly or monthly. (Table 3.10) This is higher than in Britain where only 1.6% of never smokers currently vape. (ASH 2024)
Some never-smoking vapers may have taken up smoking instead if vaping was not available. For others, vaping provides benefits such as relaxation, improved concentration or pleasure.
International surveys have found that vaping by adult non-smokers is generally less than 2%, for example Great Britain 1.6%; New Zealand no regular use; United States 0.3%; European Union current daily use by never smokers 0.08%; Germany 0.3%; Iceland 0.4%; and Greece 0.2%.
There is no evidence that vaping is renormalising smoking
Vaping critics fear that widespread vaping could make smoking appear more socially acceptable again and undermine decades of successful tobacco control efforts. However, a review of studies on renormalisation found no evidence that this is happening.
According to Public Health England , ‘There is no evidence that ENDS are undermining the long-term decline in cigarette smoking among adults and youth and may in fact be contributing to it’.
This was also confirmed in another study of adolescents in Great Britain during a period of rapid growth of vaping. Another recent review by the National Institute of Health and Care Research came to the same conclustion – youth attitudes to smoking became more negative over the time when vaping was increasing, the opposite of what would be expected from renormalisation.
The main sign that renormalising is occurring would be stagnating or rising smoking rates. In fact, the opposite is occurring. Smoking rates have declined at a faster rate in the UK and US since vaping became widely available.

Smoking at the same time as vaping is called “dual use”. This is often a temporary transition phase and is usually less harmful than exclusive smoking. However, dual users should try to quit smoking completely as soon as possible.
Some smokers quit smoking soon after they start vaping. Others take longer and smoke and vape for a period while trying to transition to exclusive vaping. Smoking while using NRT while smoking is just as common as smoking while vaping, and is a transition towards quitting.
Dual users are a mixed group. Some are predominantly smokers who vape occasionally. Others mostly vape, but smoke occasionally.
People who smoke and vape are more nicotine dependent than smokers who do not vape and are therefore likely to find quitting more difficult. (McNeill; Farsalinos)
How common is dual use?
In two recent surveys in Australia, the dual use rate was 31% [DoHA 2023] and 33% [NDSHS 2023 Table 3.41]. In Great Britain, 37% of current vapers were also smoking in 2023 and in the United States the dual use rate was 35-39% in two national surveys in 2019.
Dual use tends to decrease over time at a population level as more dual users quit smoking. In the Australian DoHA study, dual use fell from 64% in 2018 to 31% in 2022. In Great Britain dual use declined from 67% in 2013 to 37% in 2023.
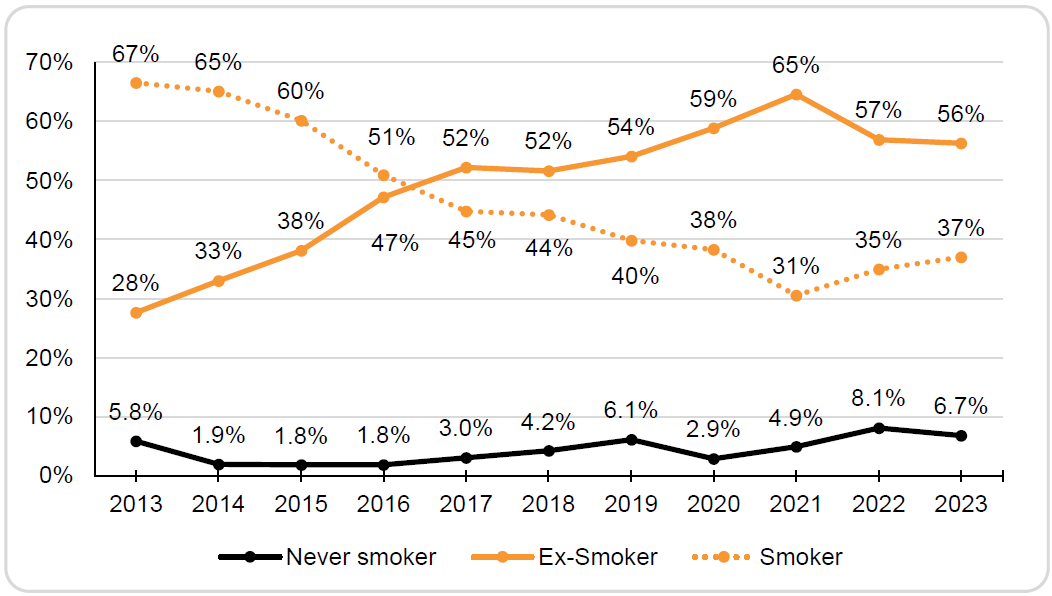
Dual use in Great Britain declined substantially over time. Source ASH UK
In a recent large study in the US, adults who purchased a Juul device gradually reduced dual use over 24 months follow-up. (Kim 2024)
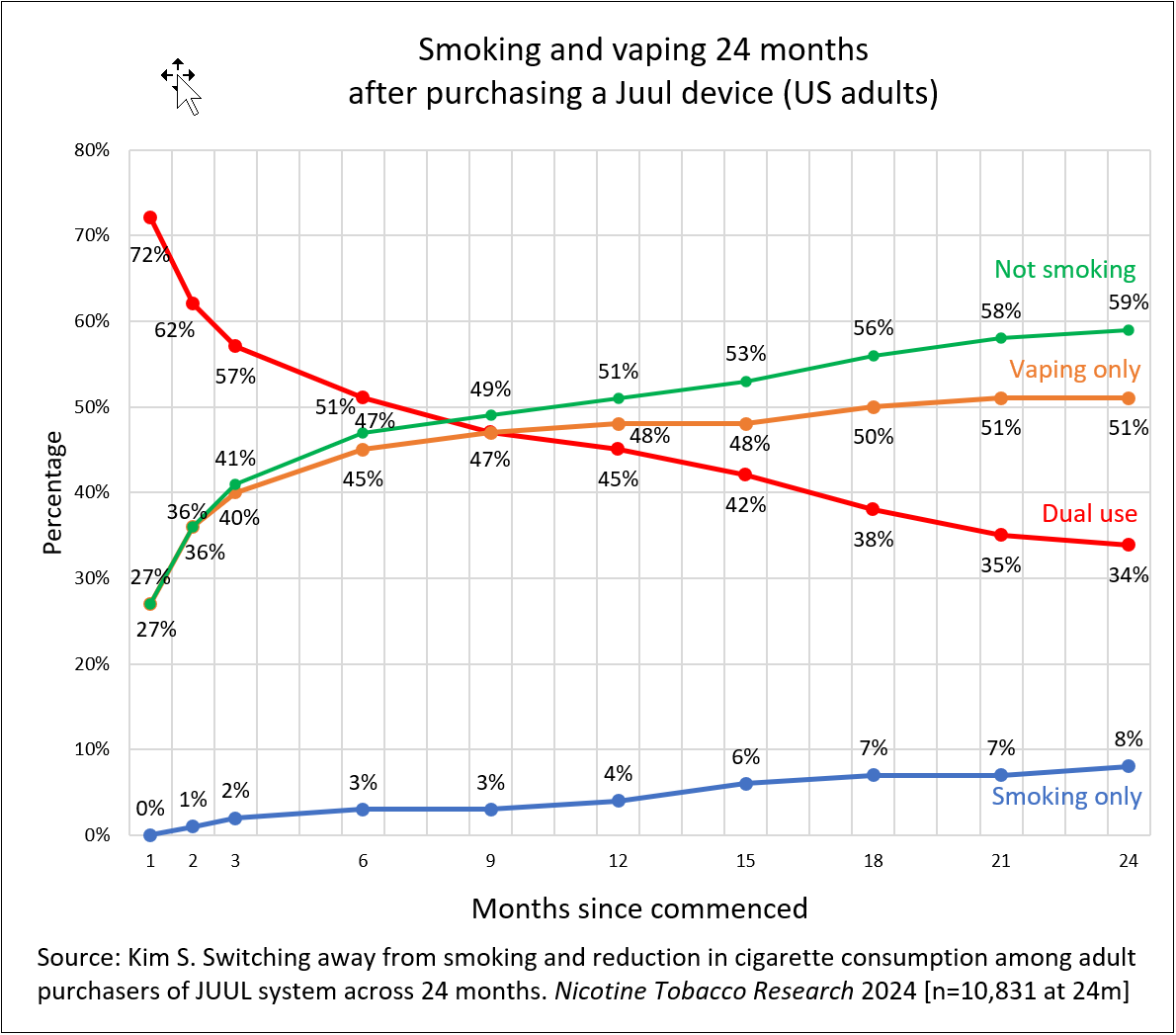
Dual use continued to decline over 24 months of follow up (Kim 2024)
Is dual use harmful?
Dual users usually reduce their cigarette intake, often to very low levels because they are getting some of their nicotine from vaping. In one study, 45% of dual users reduced their daily smoking by 50% or more. (Kim 2024) Dual users have lower levels of toxins (Hartmann-Boyce 2023) in the body compared to exclusive smokers although the improvement is not as great as for exclusive vapers. Many studies show improvements in health, such as blood pressure and asthma. However, when dual users do not reduce their cigarette intake, toxin levels are not reduced compared to smoking.
One exception is cardiovascular disease. Numerous studies have found that dual use significantly increases the risk of heart disease and stroke. (Chen; Berlowitz)
The only potential harm from dual use is if it reduces interest in quitting. However, this does not appear to be the case. Smokers who vape are more interested in quitting than those who do not and are more likely to make quit attempts.
One reason for continuing dual use is the widespread misinformation about the risks of vaping. Many people incorrectly believe that vaping is as harmful as, or even more harmful than smoking. If you believe that, why would you bother trying to stop smoking?
Quitting dual use
Dual users are more interested in quitting and are more likely to quit smoking than other smokers, especially if vaping daily. However, smokers who become dual users are often more nicotine-dependent and many will not be able to quit smoking in a given attempt. Studies have typically found that 20-45% of dual users quit smoking over the next one to two years.
A randomised controlled trial of varenicline (Champix) found it was effective in helping long-term (>12 months) dual users quit smoking. Between 4 and 12 weeks, 50% quit with varenicline and 17% with placebo.

Vaping is substantially cheaper than smoking in Australia and can lead to large financial savings.
Australia has the highest priced cigarettes in the world. The average cost of smoking in Australia is $11,860 per year (13 cigarettes per day; a 20-pack of the leading brand costs $50). Vaping costs $500-2,000 per year depending on the type of device used, a typical saving of over $10,000 per year on current prices
Under the 2024 regulations the cost of vaping will increase. Vapers now require regular doctor visits for nicotine prescriptions. The price of vapes will increase due to pharmacy markups and the additional costs of compliance for manufacturers and distributers.
This is especially important for low-income and disadvantaged populations such as people with mental illness, substance use disorders, Indigenous people, prisoners, LGBTIQ+ communities and people who use drugs whose families suffer considerable financial stress, and have less money for other essential needs like food, housing, healthcare, and education.
Disadvantaged populations have twice the smoking rate of the wealthy, smoke twice as many cigarettes and have lower quit rates. Smoking is responsible for half the difference in life expectancy between the most and least advantaged in society,
Smoking is a social justice issue and vaping could help reduce financial inequalities.
The growing popularity of vaping products has raised concerns about their environmental impact, especially from disposable products. Vaping products have a far lower impact on the environment than cigarettes because most users do not vape long-term, however they are a growing source of litter, environmental harm and fires.
Recycling of vape products is important because it
- Reduces pollution, litter and public cleaning costs
- Allows reclaiming of valuable metals such as lithium
- Reduces the fire hazard from discarded batteries
- Reduces waste and landfill
- Reduces cleaning of public spaces and beaches
Currently most disposable vapes are sold illegally on social media and at retail outlets. Recycling is not an option for these illegal sales, which are mostly disposable products. A recycling program is only workable when nicotine vaping products are made legal, adult consumer products sold from licensed retail outlets
A national recycling program
A vape recycling program is best managed by expanding the existing National Television and Computer Recycling Scheme under the auspices of the Australian Government Department of Climate Change, Energy, the Environment and Water.
The first step required is to make nicotine vaping products legally available for sale through licensed retail outlets, such as vape shops, conveniences stores, pharmacies and tobacconists. The recycling model can only be applied to the legal market.
Recycling of vape products would be mandatory for all licensed vaping product retailers. Monitoring would be required with fines and loss of licence for failing to comply with recycling rules.
How it works
The recycling process is set out in this flowchart:
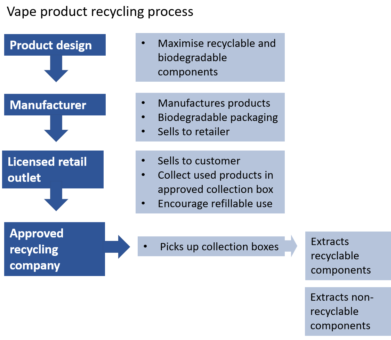
Recyclable extracts are used to manufacture other products. Non-recyclable components are disposed of in landfill.
All retail outlets selling nicotine vaping products would be licensed and have mandatory recycling boxes for used devices. Recycling boxes would be available at other locations as well.

Consumers would return used products when purchasing supplies. Consumers would need to be educated and a financial incentive could be provided, such as a small discount on future purchases.
Recycled products would be collected by recycling companies. Components would be recycled and reused.
Reading
Draft discussion paper on the environmental impact of vaping products for Australia. Sept 2023
UK Vape Industry Association. A greenprint for sustainable vaping. March 2023

Some vaping sceptics argue that there are things we don’t know about vaping, so it is better to wait until we have more information, and this could take several decades. ‘Better to be safe than sorry’. This is known as the ‘precautionary principle’.
However the precautionary principle is misused when applied to vaping in this way. When correctly applied, the precautionary principle requires a full assessment of both the potential risks and benefits of both adopting and rejecting a new product.
In the case of vaping nicotine, the risks of NOT adopting vaping are much greater because cigarettes are substantially more harmful. Banning nicotine vaping denies smokers the opportunity to quit or switch to a much less harmful product.
This requirement for long-term evidence is not applied to other products. If we applied this standard in other areas, no new medicines would be introduced until we had safety data from 20-30 years of use.
The English epidemiologist Sir Austin Bradford Hill explained that science is never complete and that waiting for final proof can cause more harm than good.
Over the past 15 years there has not been a single confirmed death from nicotine vaping anywhere in the world and serious adverse effects are extremely rare. The alternative behaviour, tobacco smoking, kills 8 million people world-wide per year.
In Australia there are about 21,000 deaths each year from smoking related conditions.
The Royal Australian and New Zealand College of Psychiatrists states in its 2018 Position Statement on vaping:
“Further research is required to ascertain the effectiveness of e-cigarettes and vaporisers as tools for smoking cessation and whether they may provide a novel route into smoking initiation. This does not justify withholding what is, on the current evidence, a lower-risk product from existing smokers while such data is collected.”
The tobacco industry

Vaping is not a ploy by the evil tobacco industry to “hook a new generation of Australian children on nicotine” as claimed by some anti-vaping activists and the Health Minister Mark Butler. This is a convenient narrative by vaping opponents to undermine vaping by poisoning it by association with Big Tobacco.
None of the disposable vapes sold in Australia on the black market and used by young people are made by tobacco companies. All of these are imported illegally from China.
In any case, vaping is diverting young people away from deadly smoking. As youth vaping rates increase, smoking rates in countries like New Zealand, the UK and US are falling faster than ever (see above)
The reality is that vaping is a huge disruptive threat to the tobacco industry and is a direct competitor to its highly profitable tobacco sales, much like digital cameras were to Kodak and electric cars are to petrol vehicle manufacturers.
The modern e-cigarette invented in 2003 by a Chinese pharmacist and industry growth has been consumer driven. The tobacco industry began investing in vaping in 2012 in response to the clear threat. It has been trying to catch up ever since and in 2022 controlled only 26.2% of the global vapour market (according to Euromonitor). BAT has a 22% share.
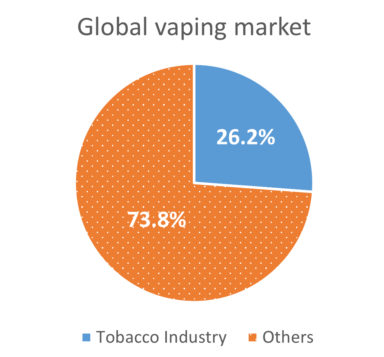
The tobacco industry is transforming
In response to the rise in vaping, the major multinationals are moving away from combustibles to much safer nicotine alternatives (like vaping, HTPs, nicotine pouches), some faster than others. PMI has gone furthest so far, spending USD 10.5 billion since 2008 in research, development, and commercialization of safer alternatives to smoking. It now earns 35% of net revenue from reduced risk products, aiming for over two-thirds by 2030 and to finally become “smoke-free”. This transition to safer products is a huge positive for public health and should be encouraged rather than obstructed.
Some skepticism is justified. Tobacco companies have lied about the harms of smoking for decades. They continue to oppose tobacco control policies and promote the sale of cigarettes. However, the transformation would be faster if activists like Professor Chapman ceased resisting it. By opposing industry transformation, he is inadvertently supporting the very thing he should be trying to eradicate – combustible cigarette sales.
But lets not kid ourselves. The push by the tobacco industry is not driven primarily by public health concerns but is a response to commercial realities created by consumer preferences. However, in this case the goals of the industry are aligned with those of public health. It’s a win-win for everyone: the industry, shareholders, consumers, and public health.
Does it matter who makes reduced risk products?
The focus of tobacco control is to prevent smokers dying from cancer, lung and heart disease. Safer alternatives to smoking will save lives, regardless of who manufactures them.
Furthermore, allowing reduced-risk options for nicotine provides an exit strategy for the industry. It may enable tobacco companies to escape from manufacturing only the most dangerous nicotine delivery system – combustible cigarettes.
Further reading: Mendelsohn CP. How opponents of vaping aid and abet Big Tobacco. The Spectator 2020

History shows that banning cigarettes doesn’t work and tobacco companies can’t be made to stop production.
Prohibition doesn’t work
Bhutan, a small country in the Himalayas, banned the sale, purchase and possession of tobacco in 2004. This led to massive tobacco smuggling, black market sales, soaring prices, a loss of taxation and an increase in smoking by both young people and adults. The ban was revoked in 2022. Attempts to ban the sale of a legal product would also inevitably lead to legal action by tobacco companies.
In South Africa, the government banned tobacco sales during the COVID pandemic. The legal supply was soon replaced with a thriving black market and substantial loss of government revenue.
Prohibition of other drugs also doesn’t make the drug disappear, it simply changes how it is supplied. In the 2023 National Illicit Drug Reporting System (IDRS) Interviews, 91% of Australian intravenous drug users reported that it was ‘easy’ or ‘very easy’ to access heroin (Figure 5). Heroin has been banned in Australia since 1953.
Nor can tobacco companies just stop production
It is naive (or disingenuous) to insist that tobacco companies stop making cigarettes. Public companies have a legal obligation to shareholders to maintain value and profits.
A Board making such a decision would be sacked and others would take its place. Even if the company closed shop, its competitors would take over and nothing would change.
In any case, there are still over a billion smokers who rely on cigarettes. If tobacco companies transition from deadly cigarettes to safer non-combustible nicotine alternatives, many will switch to getting nicotine from these less harmful alternatives.
Regulation of vaping

Nicotine liquid and vaping devices can only be legally purchased from pharmacies with a doctor’s prescription and only to quit smoking. Recreational vaping is banned. From 1 October 2024, a prescription will only be necessary for nicotine concentrations over 20mg/mL.
However, most vapers access supplies from black market sources, such as tobacconists, convenience stores, and via social media. Some vapers will go back to smoking as a result of the harsh restrictions. Here are the latest guidelines
1 July-30 September 2024
1. Eliquid
- A nicotine prescription is required from a medical practitioner. However, very few are willing to write prescriptions
- Nicotine liquid and vape devices can only be purchased legally from pharmacies. Sale from other retail outlets is banned, including existing stock
- Flavours are restricted to mint, menthol, and tobacco
- Advertising and promotion are banned including on social media
- Do-it-yourself (DIY) home mixing is banned. Only finished products are lawful to dispense. Pharmacists cannot dispense ingredients for patients to use to mix their own vaping substances
- Non-therapeutic vapes are banned ie only vapes used to stop smoking are allowed
- The importation of e-liquid into Australia for personal use remains banned
- The only vaping products that can be legally imported and sold in Australia are those whose sponsor has notified the TGA that they comply with the applicable standards.
 The list of notified products is available on the TGA website, including e-liquid refills, pod vapes, prefilled pods, refillable vapes and accessories (coils).
The list of notified products is available on the TGA website, including e-liquid refills, pod vapes, prefilled pods, refillable vapes and accessories (coils).
2. Devices
- Are now classified as medical or therapeutic devices
- Can be legally purchased only in pharmacies. A prescription is not needed. Sale from tobacconists, vape shops and convenience stores is banned.
- Single-use vapes with or without nicotine are banned (cannot be imported, sold or manufactured)
- The importation of vape products into Australia for personal use remains banned
From 1 October 2024
Nicotine liquid will be reclassified in the Poisons Standard from Schedule 4 (prescription-only medicine) to Schedule 3 (pharmacist-only medicine). From this date
- Adults can purchase nicotine liquid <20mg/mL without a prescription
- A prescription will be needed for nicotine >20mg/mL
- Nicotine liquid can only be purchased after a ‘conversation’ with the pharmacist (not the pharmacy assistant) to ensure the nicotine is for a ‘therapeutic purpose’, ie to stop smoking, and to verify you are at least 18 years old. At each visit, the pharmacist must
- Inform you that the products are not “listed or registered”
- Obtain informed consent
- Provide advice on alternative quitting aids
- Provide contact details about smoking cessation support services
- Notify the Therapeutic Goods Administration and the product sponsor if there are side effects or a defect in the product.
- Under 18s can purchase vapes with a prescription
Later
- Vapes will be sold in plain pharmaceutical packaging like medicines
- Maximum nicotine levels will be reduced
Finding a pharmacy
Finding a pharmacy selling vapes will be challenging. The Pharmacy Guild which represents the 6,000 pharmacy owners in Australia “strongly opposes the pharmacy model” and regards it as “insulting”.
TerryWhite Chemmart, Priceline, Blooms, National Pharmacies in South Australia and 777 Pharmacy Group in West Australia announced they would not supply vapes and it is likely that many independent pharmacies will also not stock vapes
Some online pharmacies are also available with a wide range of products. However, I am not allowed to tell you which ones.
Penalties
The health minister has repeatedly said that personal possession and use of vapes without a prescription will not be an offence. However, state laws allow for jail terms of up to 2 years and fines up to $45,000. This contradiction must be resolved.
For commercial offences, new maximum penalties of up to 7 years in jail and fines up to $2.2 million for individuals and $21.91 million for corporations apply.
No prohibitions apply to possession of less than a ‘commercial quantity’ of vapes.
Until 30 September 2024, the commercial quantities are [link]:
- 14 vaping devices,
- 90 vaping accessories, and
- 600mL of liquid vaping substance.
From 1 October 2024, the commercial quantities will be:
- 9 vaping devices,
- 60 vaping accessories, and
- 400 mL of liquid vaping substance.
Traveller’s exemption
Persons entering Australia by ship or aircraft may bring a small quantity of vapes under a traveller’s exemption. The vapes must be for use in the treatment of the traveller or someone the traveller is caring for, who is entering Australia on the same ship or aircraft.
The maximum allowable quantity is:
- 2 vapes
- 20 vape accessories (including cartridges, capsules or pods), and
- 200 mL of vape substance in liquid form.
Unanswered questions
Schedule 3 products (pharmacist-only medicines) are required to be registered by the TGA and listed on the Australian Register of Therapeutic Goods (ARTG). This requires an onerous and expensive process confirming safety and effectiveness. No products are registered in Australia, or in any other country. Does this mean that all non-prescription sales are now illegal?
References
The Therapeutic Goods and Other Legislation Amendment (Vaping Reforms) Act 2024
New vaping laws to commence 1 July 2024. TGA
Reforms to the regulation of vapes, 24 June 2024. TGA
TGA. Vapes: information for patients and consumers. 1 July 2024
TGA. Vapes: information for wholesale, transport, logistics and storage facilities. 1 July 2024
TGA. Vapes: information for sponsors, importers and manufacturers. 1 July 2024

Fewer than one in ten of Australia’s 1.7 million people who vape say they have a nicotine prescription from a doctor.
This figure is based on several sources
- The National Drug Strategy Household Survey 2022-23: 6.8% of current vapers age 14+ who use nicotine had “obtained a prescription” (Table 3.16)
- Independent Economics, Feb 2023 report: 8% of 393 adult vapers said yes when asked “Do you currently have a prescription to buy nicotine vaping products?” (Table 10)
- Cancer Council Victoria. October 2022 survey of 12,000 Victorian adults: “Almost 9% of past-year e-cigarette users reported that they had a prescription for nicotine from their doctor”
- Borland R, IJDP 2024. Survey in 2022: 16.5% of 158 vapers reported having had a prescription on their last quit attempt
Vaping in Australia is a criminal offence. Incredibly, the remaining 1.5 million vapers have chosen to break the law and risk substantial fines and even jail terms, to be able to vape. A prescription has been required to vape nicotine in Australia since 2012.
Why do so few people have a prescription?
These are the common reasons given for not having a prescription:
Supply
- Illicit products are so easy to access via the black market, from retail outlets, social medial, social sources and online
Doctor issues
- Difficulty finding a doctor who is willing to prescribe nicotine and is educated about vaping. Most scripts appear to be provided by online services.. Of more than 100,000 registered medical practitioners in Australia in 2023, only around 5,000 gained TGA approval to prescribe nicotine liquid
- Not wanting a lecture from the doctor about the harms of vaping
- Time consuming and inconvenient
- The cost of a doctor’s visit
- Difficulty getting an appointment in some areas. There is currently a GP workforce crisis
- An extra burden on the health system
Pharmacy issues
- Few pharmacies stock vape supplies and most have only a very small range
- Not being able to get their preferred product
- Greater cost
- Unsatisfactory products
- Limited flavours (tobacco, menthol and mint)
Ideological opposition
- People who vape do not generally support the medical model for vaping. They do not see themselves as sick and do not see the need to go to a doctor for ‘treatment’, especially as cigarettes are widely available without a prescription
- Personal autonomy and freedom of choice, resentment of government interference
Ignorance
- Many vapers are not aware that a nicotine prescription is needed
Reading
Blog. Aussie vapers speak out about the ban. 27 November 2023
Borland R et al. Do Australians use the prescription pathway when using nicotine vaping products to quit smoking? Int J Drug Policy 2024
Jongenelis MI. Perceptions of a prescription model for accessing nicotine vaping products. Health Prom Int 2023
Selamoglu M. Why do we have to be the gatekeepers? BMC Primacy Care 2024
Australia’s prescription-only regulation of vaping amounts to prohibition, or a “de facto” ban.
The essence of a ban is to prevent access or to make access so difficult that it becomes impractical for the average person to follow the preferred legal pathways. Only seven percent of Australia’s 1.5 million adult vapers who use nicotine reported having obtained a prescription for nicotine and source supplies from the black market – a clear indicator of the disconnect between legislation and the real-world behaviours of consumers.
The restrictions on legal access include:
- Very few doctors are willing to write prescriptions for nicotine
- The process of getting a prescription is costly and inconvenient and has been rejected by most vapers
- Very few pharmacies stock vapes and those that do have a very small range
- Regulatory and pharmacy markups have substantially increased the price
- Many vapers have a preferred device and flavour, often after experimentation over some time. The preferred product is unlikely to be available from pharmacies
- Most of the products available on prescription are unappealing. They are only available in tobacco, menthol and mint flavours
- Later this year, the nicotine concentration is likely to be reduced to 20mg/mL, which is far too low for many vapers
This is in sharp contrast to deadly cigarettes, which are freely available over-the-counter from up to 40,000 retail outlets. in Australia.
A “Clayton’s” prohibition
Make no mistake. While Australia’s vaping regulations may not constitute a ban in the strictest legal sense, it has all the classic hallmarks of prohibition [link]:
- The market is controlled by criminal networks
- Criminal gangs are engaged in a turf war to control the market with widespread firebombings and killings
- Profits are laundered and used to fund other criminal activities
- Products are unregulated and less safe
- Vapes are freely sold to youth
- Law enforcement is essentially ineffective and there is widespread and easy access
Arguments that harsh vaping regulation is not prohibition rest on the flawed assumption that if people who vape can acquire a medical prescription, then vaping products are not ‘prohibited’. This argument is inaccurate.
Alcohol was also available on prescription during the prohibition of alcohol in the US from 1920-1933. However, like vaping in Australia, most consumers sourced their supplies from the illegal market. Prohibition was a huge failure and led to unintended consequences, such as increase organised crime and corruption, smuggling, bootlegging of dangerous and stronger alternatives, overloading of the courts and prisons, and loss of tax revenue.
History has taught us that banning a popular product does not cause it to disappear. Instead, it drives it underground, criminalises users and exposes them to additional risks from dangerous, unregulated products and exposure to criminals.
Prohibition doesn’t work
Prohibition of large-scale and established black markets are very rarely successful. This is because when demand for an illicit good is high, as is the case with non-prescription vapes in Australia, it is not possible for law enforcement interventions to be mounted at such a scale as to sufficiently undermine the profitability of groups engaged in supply.
Large-scale crackdowns are not effective. Criminal groups which specialise in evading government controls will adapt and continuing supplying their customers by whatever means available, as is the case with other illegal drugs which are generally cheaper and more readily available than ever.
Even when large-scale and sophisticated criminal networks can be disrupted, the promise of extraordinary profits mean that there are always new criminal actors ready to step in and supply the market.

Flavours are integral to the success of vaping as a quitting aid for adult smokers and as a safer alternative to smoking. However, the Australian government has banned all flavours except tobacco, mint and menthol to reduce youth vaping.
E-liquid bans do more harm than good. Research shows that flavour bans increase youth and adult smoking, illicit markets and potentially dangerous workarounds.
Youth vaping
Bans on flavours may increase youth smoking as vapes and cigarettes are substitutes. For example, a ban on flavoured tobacco and vaping products in San Francisco in 2020 resulted in a more than doubling of smoking by high school students.
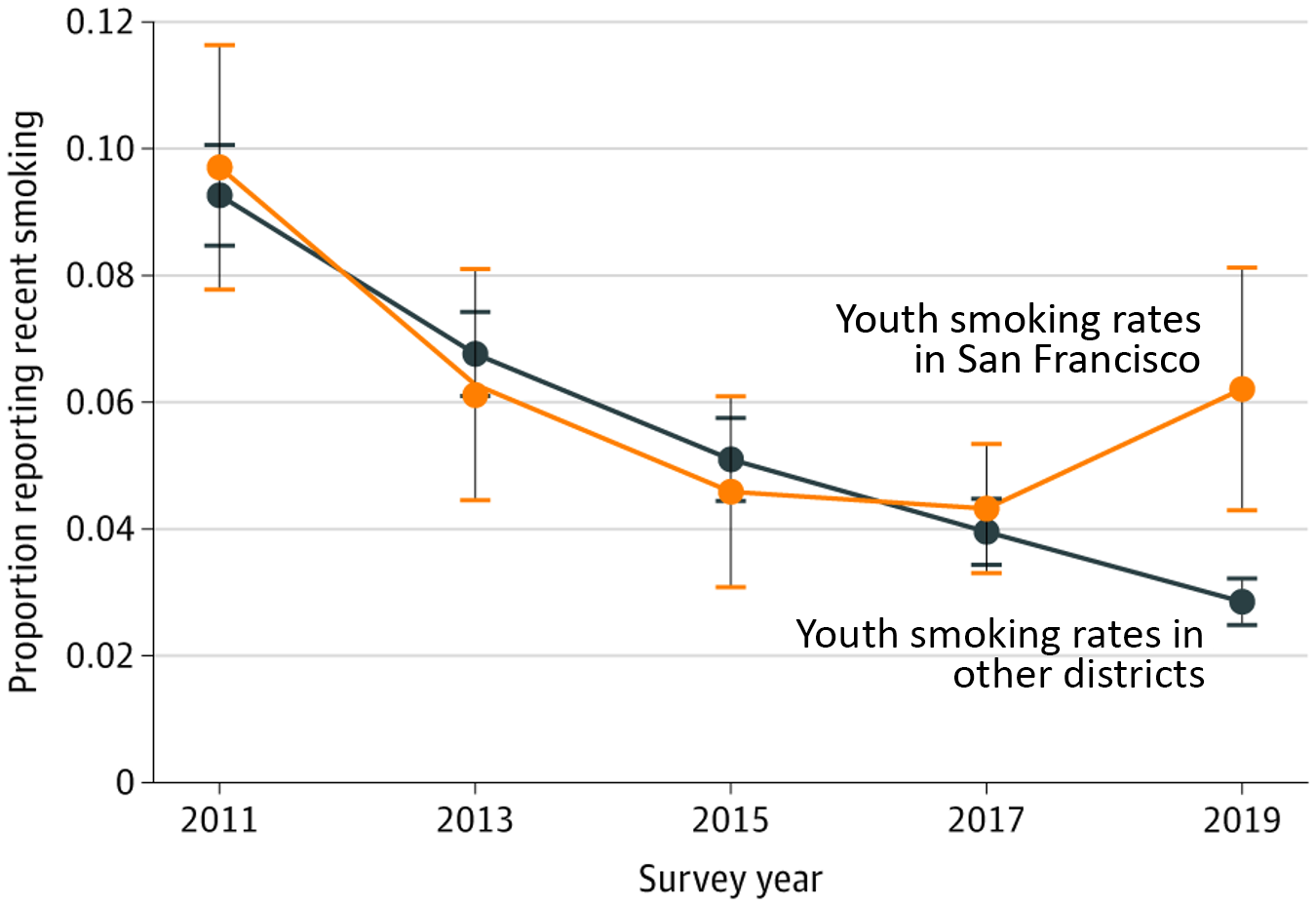
Other studies in the US have found that bans on flavours had no effect on youth vaping and users simply switch to other available options or devices and continue flavour use. (Kasza 2023; Selya 2023)
Flavours are not the primary reason for youth experimentation with vaping in Australia, the US, Canada or the UK. The main reasons kids give for vaping are curiosity, peer pressure and stress relief, followed by liking the flavours. Young people enjoy flavours but they only appear to play a small role. In a recent youth study, flavours were the eighth most common reason for use (Weinstein).
Non-tobacco flavours preferred by young people are very similar to those preferred by adults. The most popular flavours used by adults and youth are fruit, dessert, and other sweet flavours. As a result, flavour bans to protect youth are likely to be harmful for adult smokers and vapers.
Impact on adults
The likely outcome of a flavour ban is the holy trifecta of (Bates)
1 More adult and youth smoking as a result of reduced quitting, increased relapse, and decreased diversion
Flavours are an integral part of the appeal of vaping for adult smokers (Gendall; Gravely; Gades) and play an important role in the initiation of vaping for current smokers. Many smokers start vaping with tobacco flavours, but most migrate to non-tobacco flavours over time.
Flavoured e-liquids also are associated with a greater chance of making a quit smoking attempt, higher quit rates compared to non-flavoured e-liquids, smoking reduction and reduced relapse. (Glasser 2020; Li 2021; Mok 2022; Friedman 2020; Higgins 2024)
A review by the Cochrane group did not find clear evidence of an association between flavours and quitting, however this reflected an absence of sufficient evidence. (Lindson 2023)
There is strong evidence that vaping functions as a substitute for smoking. Restricting flavours leads to more smoking overall. For example, a recent large US study across 7 states and 375 localities, found that for every vape pod not sold due to flavor restrictions, there were an additional 15 cigarettes sold. As smoking is so deadly, even a small increase in smoking will lead to a net harmful effect from a flavour ban.
In surveys of vapers, most would continue to vapef flavours were banned. However, some adults (eg Buckell; Khouja; Posner; Gravely) and 12.5% of young adult vapers would switch back to smoking, a far more harmful alternative. In another study in Massachusets, flavour restrictions was found to reduce youth vaping and smoking.
Flavours are used in nicotine replacement products for this reason. Nicorette gum is available in Australia in fruit, mint, spearmint and icy mint flavours and research shows that flavoured nicotine gum enhances appeal and improves compliance.
2 Increased illegal trade in banned flavours or flavour ingredients
Flavour bans would lead to increased black-market supplies (here and here). In one study, 50% of vapers said they would find a way to buy their preferred flavour if it was banned.
Illicit products are provided by criminal networks, are unregulated with unknown potency and safety risks. This resulted in the deadly outbreak of EVALI in the US. The use of 6-methylnicotine is another potentially risky product used as a substitute to circumvent a nicotine ban.
3 Potentially risky workarounds such as home mixing for personal use and to sell to friends and acquaintances
After a ban on all flavours other than tobacco in Finland, the use of prohibited flavours remained common. Some vapers used food flavours, others purchased flavoured e-liquids online. Vaping rates did not decrease.
Safety of flavours
Flavour chemicals are food-grade and are approved for ingestion, but not for inhalation. There has been little research on inhaled flavours so far. One review of 30 studies reported that cinnamon, strawberry and menthol flavours had adverse lung effects compared with other flavours in laboratory tests. However the UK Royal College of Physicians report in 2024 stated
“Although the routes of flavour exposure from e-cigarettes and foods are different, the systemic toxicological effects will be the same for equivalent concentrations once flavourings are absorbed by the body”
According to Public Health England, “To date, there is no clear evidence that specific flavourings pose health risks but there are suggestions that inhalation of some could be a source of preventable risks”. These flavourings include diacetyl, cinnamaldehyde and benzaldehyde and should be avoided.
Suggested regulations
- Allow simple descriptions of flavour profiles only e g ‘mint’, ‘blueberry’, ‘tobacco’, ‘vanilla tobacco’
- Prohibit descriptive flavour names, images and packaging that specifically appeal to youth eg ‘dragon vomit’
- Prohibit flavours found to have a known risk to health
Reading. Farsalinos K. The case for flavors in tobacco harm reduction, to save lives. 2023
 The importation of disposable vapes into Australia was banned from 1 January 2024. However, the vast majority of disposables available are black-market disposables are already banned and a further ban is likely to have little effect on long-term supply and use.
The importation of disposable vapes into Australia was banned from 1 January 2024. However, the vast majority of disposables available are black-market disposables are already banned and a further ban is likely to have little effect on long-term supply and use.
An estimated 120 million illicit disposable devices are imported each year by organised crime gangs from China and are freely sold from retail outlets, social media and online to adults and young people. They are most popular among young adults.
The ban on disposables is mainly driven by a moral panic about youth vaping. But we also need to consider the harms of a ban on adult smokers.
A ban will increase deadly smoking
Many of Australia’s 1.6 million adult vapers rely on vaping to stay smoke-free, and some disposable users will return to smoking if their preferred product is not available – a catastrophic consequence for public health. For example, vape bans have been linked to increased cigarette sales in the US. Because of the much greater risks associated with smoking, it would take only a small uptake in smoking to make the effect net negative for the population as a whole. A UK study of 16-20-year-olds who vaped disposables and smoked suggested that a ban on disposables, strict regulation or increased prices could lead to an increase in young adult smoking.
Also some people who have never smoked but who are currently vaping disposables and are nicotine-dependent may switch to deadly smoking to get their nicotine fix.
Disposable vapes are a popular entry device for adult smokers to vaping. They are relatively inexpensive and easy to use and can make the transition from smoking a smoother process. They are also popular for smokers with severe mental illness, homelessness, learning disabilities, hospital inpatients and older smokers who struggle with more complex devices. A ban may have a disproportionate impact on disadvantaged groups that have higher smoking rates and typically find it harder to quit.
Another concern is that the ban may signal that vapes are more harmful than cigarettes, which are not banned, and could discourage smokers from switching to the safer alternative.
Other adult smokers who may wish to try disposables to quit in the future, will have reduced access. This may slow progress in driving down smoking rates by removing a popular and effective option.
Kids who want to use nicotine will most likely use another nicotine product instead. For example when flavoured pods were banned in the US, many young people simply switched to disposables.
A ban will be ineffective
As we have already discovered, bans don’t reduce access or supply, They simply transfer control to the black market suppliers who sell untaxed, dodgy products happily to young people.
According to Professor Nicole Lee from the National Drug Research Institute at Curtin University, “Banning or restricting vaping could actually do more harm than good. Banning drugs doesn’t stop people using them. Prohibition does have a number of unintended consequences, including driving drugs underground and creating a black market or increasing harms as people switch to other drugs, which are often more dangerous.”
Deakin University criminologist Dr James Martin agrees. He believes a crackdown could further fuel the black-market. “When there’s demand that strong there will always be supply that will emerge.”
Bans also lead to workarounds. When the US FDA restricted the sale of flavoured pod devices, the sale of disposables skyrocketed and has been a public concern ever since with no net benefit.
The Border Force can’t help
The Australian Border Force (ABF) is simply not equipped to intercept the high volume of illicit disposables already entering the country. According to ABF chief, Michael Outram, “banning vapes at the border won’t be enough to stamp out a rampant black market”. The ABF was already only managing to detect only a quarter of illicit drugs making their way into Australia, “even on a good day”.
Each year, 8 million shipping containers are imported into Australia and only 101,500 containers (1.3%) are scanned. A measly $25 million has been allocated to the ABF to detect vapes over the next 2 years, but their main priority is dangerous illicit drugs and firearms.
What about the environment?
Over 90% of vape litter is from black-market disposable products over which there is currently no control. Vape litter will continue if disposables are banned, but are still used widely. However, if vaping products are made legal, adult consumer products, a national, manufacturer-funded recycling program can be introduced. Almost all of the parts of modern legal disposables can be recycled.
As well, users of disposable devices should be encouraged to switch to reusable devices where possible.
What needs to be done?
Banning a product because it is sometimes consumed by people who are already banned from buying it is a poor basis for policy. A more nuanced approach is needed. The solution is to address the cause of the problem, the current restrictive, prescription-only regulation of vaping products. Getting a prescription is onerous and inconvenient, and the black market has stepped up to provide a simple and cheap alternative.
The only way to eliminate a black-market is to replace it with a legally regulated one.
Nicotine vaping products should be reclassified as adult consumer goods like cigarettes, to bring Australia into line with all other western countries, such as the UK, NZ, US and Canada. Nicotine vapes could then be sold from licensed retail outlets with strict age verification at the time of purchase with harsh penalties and loss of licence for under-age sales, strict compliance measures and spot checks.
Other restrictions to reduce uptake by young adults could include packaging restrictions, display restrictions and modest taxation.
Under this model, the black-market would become less profitable, illicit sales of disposables would diminish over time. Teens would have reduced access to vapes and adult smokers could readily access regulated products to help them quit and stay quit, including with high quality disposables.
Reading
Why Australia should not ban disposable vapes. Blog July 2023
A Vapid Solution. Why banning disposable e-cigarettes would be a failure of law-enforcement. Institute of Economic Affairs UK, Sept 2023
Will the war on vaping result in more harm? Drug Science UK February 2024

There is no justification for banning public vaping on health grounds. Secondhand vapour is an issue of public nuisance, like loud conversations on mobile phones or strong perfumes.
Exposure can be reduced by educating vapers about vaping etiquette and to be considerate of the people around them. Vapers should not blow large clouds in crowded areas or vape around children. Authorities can erect signs reminding vapers to only blow small clouds and be considerate of others.
Vaping is a ‘victimless crime’ and causes no known harm to others. Regulators should consider the harm principle, which is that “The only purpose for which power can be rightfully exercised over any member of a civilised community, against his will, is to prevent harm to others.”
A blanket ban on all public vaping sends the misleading message that vaping is just as harmful as smoking. This could deter smokers from switching to vaping. The opportunity to vape in places where smoking is prohibited is an incentive to switch to the healthier behaviour. Vapers may be more likely to relapse if they are forced to vape in smoking areas with smokers.
However, restrictions are appropriate in some circumstances, such as at schools and hospitals. It is also reasonable to disallow vaping in private homes to reduce the risk of young people starting vaping.
Public Health England recommends that vapour policy be set by owners, employers and managers for local premises according to their circumstances, rather than a blanket ban.
Potential disadvantages of vaping inside are that it might encourage people to start vaping, increase dependence and discourage vapers from quitting. A recent study found that indoor vaping restrictions increase infant mortality by 12.9% compared to locations where vaping was not restricted, most likely because restrictions led to more smoking and more secondhand smoke. (Cooper 2024)
Pharmaceutical-like plain packaging has been proposed in Australia to reduce the appeal of vapes to young people. However, this may result in increased smoking in young people and adults.
Plain packaging is appropriate for deadly cigarettes. However using it for vaping products falsely implies a similar high risk, and may discourage adult smokers from switching. Harm perceptions about vaping are already exaggerated. Most people incorrectly think vaping is at least as harmful as smoking or more harmful. Plain packaging may reinforce this misperception and deter some smokers from switching to the far safer alternative.
In young people, there is some evidence that plain packaging may reduce interest in vaping (Simonavicius; Taylor). However, vaping is diverting young people away from smoking and is helping some young smokers quit. Plain packaging may undermine that progress and may increase smoking rates as vaping and smoking are substitutes.
A better solution is make packaging simple, without bright colours or images with youth appeal (as for Juul below). Flavour names that specifically appeal to young people such as ‘dragon vomit’ should be banned and only simple flavour descriptors such as caramel or blueberry used.
Plain packaging for vapes is mandatory in some countries such as Denmark, Israel and Finland.

Four to six percent nicotine (40-60mg/mL) is a realistic upper limit for nicotine vaping liquids (depending on the device).
Vaping products need to deliver sufficient nicotine to compete with and replace cigarettes. Excessively low limits on nicotine concentration will make them ineffective for some users.
The nicotine limit of 2% proposed for Australia is too low to act as a satisfying alternative for a cigarette, especially for more dependent smokers. The selection of this level by the EU in 2014 was arbitrary and not based on any scientific argument.
Higher levels are more effective
Higher nicotine concentrations are more effective initially for quitting, especially for more dependent smokers (eg here, here, here). A nicotine concentration of 4-6% (40-60 mg/mL) is needed to match the nicotine delivery from a cigarette (depending on the device). (eg here, here, here, here)
After having quit, vapers tend to reduce their nicotine concentration over time.
Low nicotine levels will make compact pod and disposable products less effective. These devices have low-power batteries and low aerosol volumes and require higher nicotine levels, in the range of 2-6%. These are transition models for many smokers as they are easy and convenient to use and have a low initial outlay. They are especially useful for people with mental illness, for institutional use, the elderly, the homeless and the technically challenged.
Reducing the nicotine concentration will make vaping less satisfying and some vapers will return to smoking. Others will source high nicotine supplies from the black market. This has long been a problem for nicotine replacement products which fail to delivery adequate nicotine levels and craving relief and therefore have low success rates.
Higher levels are safer
When the nicotine concentration is too low, vapers compensate by more and larger puffs to get sufficient nicotine. As a result, they inhale more toxic chemicals.
Low powered devices using higher nicotine concentrations are also safer because they have lower operating temperatures, and produce fewer toxicants from thermal breakdown of the e-liquid components.
Excessively low levels of nicotine will also lead some vapers to home-mixing, purchasing high nicotine liquids (10-20%) for mixing with other ingredients. These concentrated solutions are potentially toxic, especially for small children and have led to deaths from overdose.
Trying to control nicotine exposure by reducing nicotine concentration is counterproductive and is like trying to control alcohol consumption by limiting the strength of drinks available.
What about adolescents?
There is a genuine concern about higher nicotine levels for adolescents. Higher nicotine concentrations potentially increase the risk of dependence. However, dependence by never-smokers who vape is very low.
Never-smokers who vape high levels of nicotine may initially experience nausea and dizziness. These side-effects are unpleasant but not serious.
Maintaining a low nicotine limit out of exaggerated concern for illegal use by adolescents is poor policy and will reduce the success of vaping as a quitting aid for adults.
Any regulatory measures to control youth vaping should focus on reducing access and appeal to young people. The preferred model is a strictly regulated adult consumer market with sale through licensed retail outlets with strict age verification.
Basic minimum standards for all vaping products came into effect in Australia on 1 October 2021 (updated January 2024), the Therapeutic Goods (Standard for Nicotine Vaping Products) Order 2021 (TGO110).
E-liquids
The standards specify a range of labelling, packaging, ingredient, nicotine concentration and record-keeping requirements for nicotine e-liquids. The standards regulate nicotine as a medicine and include the following requirements:
- The label or information sheet must state the nicotine concentration in mg/mL and a list of all ingredients
- The label or information sheet must state ‘KEEP OUT OF REACH OF CHILDREN’, ‘Avoid contact with eyes’ and ‘Avoid contact with skin’
- Prohibition of 2,3-pentanedione, acetoin, benzaldehyde, cinnamaldehyde, diacetyl, diethylene glycol, dl-alpha-tocopheryl acetate, ethylene glycol
- Nicotine
- Maximum concentration of 100mg/mL (to be reduced from 1 October 2024(
- The concentration must be within 10% of what is stated on the label
- Nicotine must be the only active ingredient
- Only tobacco, mint, menthol flavours
- Child-resistant container
Vaping devices and accessories
From 1 March 2024, all vaping devices and accessories (including an unfilled cartridge, capsule, pod or other vessel) are covered by the therapeutic goods framework and are required to comply with one or more of the following:
- The Essential Principles, or
- where applicable, the Therapeutic Goods (Medical Device Standard—Therapeutic Vaping
Devices) Order 2023 (the MDSO)
Reference. Therapeutic Goods (Standard for Nicotine Vaping Products) (TGO 110) Order 2021 (updated 2024)

Taxation on vaping products should be kept to a minimum to encourage smokers to switch to the safer product.
There is a good case for high tobacco taxes on cigarettes to discourage their use and reduce smoking rates. However, vapes are a less harmful substitute for smoking and there is no justification for high taxes on health grounds. Low taxes on vaping will provide an incentive to smokers to switch and will improve public health.
Vaping nicotine should be taxed according to risk. Vaping is at least 95% less harmful than smoking and the tax level should reflect that low risk. The tax rate for vapes in the UK and New Zealand is 15-20%, in line with the GST or VAT.
Furthermore, smoking is increasingly concentrated in low-income and disadvantaged groups and this is the population at greatest risk. A significant tax differential between vaping and smoking should be maintained to incentivise switching to the less harmful alternative, especially for this population.
Increased taxation of vapes has led to increased smoking by youth (here and here), young adults, adults. and prenatal and pregnant women. This suggests that vapes and cigarettes are economic substitutes.
One modelling study found that every 10% increase in e-cigarette prices was associated with a drop in adult e-cigarettes use by up to 11.5% and was associated with a significant increase in smoking.
Because the benefit to society is so high, regulators should look to other sources of income to replace tobacco taxes. Raising vape taxes to replace tobacco excise is as illogical as saying that someone who switches from driving a car to riding a bicycle should expect new taxes on biking to replace the lost petrol taxes.
Taxation on vaping products should be kept to a minimum to encourage smokers to switch to the safer product.

A blanket advertising ban is counterproductive. Advertising can help to raise public awareness about new options to replace deadly smoking and motivate smokers to try to switch. Advertising bans on much-safer entrant products would protect the established cigarette trade from competition.
Responsible adult-orientated advertising would restrict the content, timing and placement of advertising so that it is appropriate for adult audiences and communicates the relative risk compared to smoking.
- Restrict advertising targeted at smokers who are unable or unwilling to quit with a ‘switch’ message.
- Ban all advertising that could appeal to young people, such as lifestyle ads associating vaping with positive imagery and adventure.
- The placement of advertising to minimise exposure to young people.
The attempt to strike a pragmatic balance between promoting products that provide significant benefits to adults while controlling the effect on adolescents has been addressed in the UK Code of Advertising Practice that applies to UK domestic advertising for e-cigarettes.

Vaping products are consumer products and should be regulated by the Australian Competition and Consumer Commission (ACCC) which provides strong protection for consumers.
Vapes were originally developed as a less harmful consumer alternative to deadly combustible cigarettes (another consumer product), to reduce harm for smokers who are unable or unwilling to quit. They are largely used for this purpose. However, vapes also provide other benefits and are used in some cases as ‘recreational’ products, for example for pleasure, social benefits, relaxation and improved cognition.
Vapes are not medicines. They are not a treatment to manage a health condition and do not require medical supervision. People who vape do not regard themselves as sick, requiring medical attention. No other country requires vapers to have medical management or to have a nicotine prescription.
Vapes should not therefore be regulated by Australia’s medicines regulator, the Therapeutic Goods Administration (TGA). The TGA is responsible for regulating medicines and medical devices which make therapeutic (medicinal) claims, such as ‘this product can help you quit smoking’.
No country requires vaping products to undergo medicines regulation. It makes no sense to require the highest medical standards of research and quality for nicotine vapes when they are replacing a far more harmful product, lethal cigarettes, which are virtually unregulated. No vaping products are classified as medicines by the regulator in any other country.
For a medical classification, every device and e-liquid and every future modification would require a detailed, costly and onerous application that only tobacco companies could afford. Most small to medium companies and vape shops would be driven out of business. The result would be that tobacco companies take over the vaping market.
The ACCC can ensure that products are safe, fit for purpose, of merchantable quality and comply with all legal requirements under the Competition and Consumer Act 2010.
